Click Here to Download PDF Version
Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
| What is New?
The Personal Data Privacy act has been long overdue in India. It was introduced in the parliament in December 2021, to regulate personal and non-personal data jointly but was withdrawn in August 2022. The government has now put out the draft of the telecommunication bill that was put out recently for public comments (https://dot.gov.in/relatedlinks/indian-telecommunication-bill-2022). Comments may be sent on the email ID : naveen.kumar71@gov.in Last date of sending the comments will be 20th October 2022. This bill will influence the provisions in the data privacy act too. The existing regulatory framework for the telecommunication sector is based on the Indian Telegraph Act, 1885. With advent of new technologies such as 4G and 5G, Internet of Things, Industry 4.0, M2M Communications, Mobile Edge Computing, AI and many more, the technologies are creating newer opportunities for India’s socio-economic growth. Therefore, India needs a legal framework attuned to the realities of the 21st century. The draft bill covers conventional phone calls, text messages broadband connections and over-the-top applications, including WhatsApp defined as telecommunication services. The worrying aspect is that the bill seeks the regulatory powers to control and management of, or suspending the operation of services without putting a review mechanism in place. The explanatory note to the bill says – “The Bill provides an enabling framework for the Central Government to address any situations of public emergency, public safety, or national security concerns. These provisions provide for the time-bound limited suspension of transmission of messages, or of provision of telecommunication networks or services while ensuring the rights of the citizens of India,” The Supreme Court in January 2020 had said that such shutdowns should be temporary and periodically reviewed. No review mechanism has been mentioned in the draft bill and this will invite criticism. Such provisions will have a bearing on the Data Privacy Act too. The Sept Newsletter covers an updated information on Data Privacy Act from Ms. Bagmissikha Puhan. It is now just another 6 weeks to the national conference of TELEMIDICON2022 at Kochi. Do register in large numbers to make this national event a success. Wish all our members a Happy festivities during Navaratri. Thank You |
 Digital India Act and Pending Legislations
Digital India Act and Pending Legislations
Bagmisikha Puhan
Associate Partner, TMT Law Practice
Siddhant Gupta
Associate, TMT Law Practice
The Data Protection Bill, 2021, introduced in December 2021, to regulate personal and non-personal data jointly, was withdrawn in August 2022, in view of the increased regulatory compliance upon start-ups, and persistent opposition from stakeholders on provisions of data localization, data transfer, and LEA access to such datasets [including anonymized data]. The absence of a comprehensive data privacy legislation compels stakeholders to rely upon sectoral guidelines, which while enforceable, may become more onerous, for want of a common thread across all sectors. It is expected that the Information Technology Act, will also undergo a complete overhaul, pending legislation with respect to data privacy . The intention of legislature is to create a future-proof, comprehensive regulatory landscape for the regulation of digital activities, the government has proposed to issue a set of legislations, to usher a comprehensive framework for information technology law and regulation.
The legislators propose to introduce the Digital India Act (DIA), to address the convergence in technologies, services, and devices in the digital ecosystem. The DIA is expected to govern aspects of regulation of intermediaries, over-the-top (OTT) platforms, and provide for guidelines around women and child safety on the internet. While the DIA is expected to be tabled in the winter session of the Parliament, the privacy legislation may be introduced only during the budget session.
Presently, the regulation of over-the-top platforms is not contemplated under any enforceable statute; DIA is likely to provide for a definitive classification for OTT services, and provide guidelines for developing appropriate self-regulatory methods, providing guidelines around classification of content, age verification mechanisms and other issues.
DIA is further expected to account for new age technologies, such as artificial intelligence, internet of things, blockchain, and address regulatory concerns. Keeping in mind the business friendly outlook of the regulators towards digital space, it is expected that there would be an evaluative criteria to determine the level of compliance for entities. With the existing telemedicine practice guidelines referencing the usage of AI, ML, and big data to the advantage of the platforms, as well as the practitioners, a little more clarity will drive the functionality of platforms in the digital health sector, better. Interestingly, the telecom regulator is also considering revisions around use of this technology in the telecom sector, which will be also something that the digital health world will rely upon.
It is expected that DIA will harmonize the legislations, regulations, amendments released within the last couple of years, with respect to social media platforms, digital services, and blockchain related business undertakings. Towards such end, the government had released a draft Non-Personal Data Governance Framework in 2021, for consultation, to enable controlled access to non-personal data for “sovereign, public good purposes”.
It is expected that the DIA shall provision for such controlled access to NPD, per the granularity criteria of DIA, to provide access to such aggregated data sets to public, private entities, for their intended use. It is pertinent to note that IRCTC had sought to capitalize on the passenger sets available and had introduced a tender for hiring consultants in order to formulate a passenger data monetization plan. For example, businesses may have access to estimated footfalls in a particular location based on ticketing volumes bound for the location through IRCTC’s monetized data. The scope of work was to be limited to sharing aggregated data and anonymous data for sharing with private and government companies; however, in absence of a dedicated central data privacy legislation, the tender has been temporarily put under review.
1. https://indianexpress.com/article/opinion/columns/why-we-need-to-build-a-framework-for-global-digital-governance-8160848/;
2. https://www.moneycontrol.com/news/business/drafting-of-new-data-protection-bill-almost-complete-as-centre-to-introduce-it-in-parliament-by-budget-session-ashwini-vaishnaw-9197031.html
 TSI Mid-Term Conference – Proceeding and Recommendation Thereof
TSI Mid-Term Conference – Proceeding and Recommendation Thereof
Mr. Farooq Ahmad Wani M. Tech.
Superintending Engineer, Electronics & Communication / Information Technology (E&C/IT),
Sher-i-Kashmir Institute of Medical Sciences (SKIMS), Soura, Srinagar | State Nodal Officer (Telemedicine), Jammu & Kashmir
Department of Electronic Communication & IT at Sher-i-Kashmir Institute of Medical Sciences or SKIMS conducted the first TSI Mid-Term Conference 2022 in Jammu and Kashmir under the Aegis of Telemedicine Society of India on 25TH – 26TH AUGUST, 2022.
The Chief Guest of the Conference was Shri Rajeev Rai Bhatnagar, Advisor to Hon’ble Lieutenant Governor J&K and the Guest of Honour was Shri Bhupinder Kumar (IAS) Administrative Secretary, H& M E Department, J&K. The event was attended by faculty SKIMS, faculty from other Institutions, Administrative staff and students along with the national TSI executive members.
This event in Srinagar holds special significance as it is the first of a kind conference in this UT and this could give great impetus to the ongoing rolling out of ABDM in the UT.
As far as Telemedicine in J&K is considered, the Government of Jammu and Kashmir and The Indian Space Research Organisation (ISRO), both have contributed immensely to creating this facility at SKIMS along with 12 other Medical Colleges/District & Sub District Hospitals with SKIMS Telemedicine Centre as its hub.
Theme
The theme of the event had been carefully chosen – “Telemedicine in Special Conditions & Special Geographies” as we expected that the conference became a platform for discussing the role of Information Communication Technologies (ICT) in bridging the gap between the patient and the doctor in the terrains like J&K.
The theme was apt for the UT as it is a disaster-prone area and has the occurrence of earthquakes and floods, and turmoil prone. It also has extreme winter, making many of its parts inaccessible during winter periods. This is particularly true for Ladakh, Gurez, and Zanskar areas and some parts of the Jammu region which include Padar and Wud Vun, that remain cut off for more than six months in a year.
Telemedicine has the potential to play a bridging role in overcoming these challenges. Telemedicine also finds its use in places where large populations occasionally/periodically gather at a point in time, where the provision of medical care becomes the need of the hour; for example, the Government of J&K practices telemedicine during the Amarnath Yatra.
The Chief Guest along with the guest of honour inaugurated the two-day mid-term conference in presence of various other dignitaries.
Key Messages from the Dignitaries
- Shri Rajiv Rai Bhatnagar who was the chief guest on the occasion in his address complimented SKIMS for pioneering services in Telemedicine. He said there needs to be more focus on telemedicine services in UT J&K attributing vast expansion in the medical area. He also said that critical services need to be accessible in remote places and access to masses to various services in telemedicine needs to be prioritized. He hoped that today’s event will provide us with better inputs and ideas to further improve upon the better patient care services.
- Mr. Bhupinder, IAS, Secretary Health and Medical Education Govt. of J&K who was the guest of honour on the occasion said UT J&K has many inaccessible areas and has made a lot of strides to adopt digital services and the general public has been provided satisfactory services like comprehensive call centres, mobile ambulances in remote areas. He further said IT solutions including hospital management system are revolutionizing the functioning of hospitals. He underlined that user-friendly technology can be significant in the use of telemedicine services and emphasized training/capacity building of practitioners and said a lot more needs to be done to popularize telemedicine services to benefit the common man. He also highlighted various services being provided under the Ayushman Bharat Initiative in UT J&K including Ayushman Bharat Pradhan Mantri Jan Arogya Yojana. He said times like COVID made the adoption of technology much easier and brought greater work efficiency and the use of various applications generating sufficient data helps strategize policies for the future to come.
- Director SKIMS Prof. Parvaiz A. Koul complemented the organizing team and thanked the Telemedicine Society of India for choosing SKIMS for the event and said that SKIMS is the only public hospital with a well-established Telemedicine Centre and said the department of Electronics and Communication/IT needs to be commended for their excellent work. He further said SKIMS recently digitized important service areas including patient registration, payment system, and report access which has been well received by the public and has facilitated patient care services here at SKIMS.
- Prof. Tariq Gojwari, Dean Medical Faculty and organizing chairman, while speaking on the occasion gave a detailed account of Telemedicine services at SKIMS and said SKIMS is the only tertiary care centre with well networked digital platform which has so far benefitted the huge number of patients.
- Prof. Prasanta Kumar Pradhan, President of the Telemedicine Society of India who joined online while addressing the audience said that it is the first mid-term conference organized by the Telemedicine Society of India in J&K. He emphasized the use of digital technology in health services. India has adopted digital technology which has been a game changer and has brought greater accountability and accessibility to health care services, he added.
- Dr Murthy Remilla LN, Hon. Secretary TSI, welcomed the dignitaries and the guests. At the outset he, complemented the Director SKIMS for allowing the conference at such short notice. He urged, not to see the quantity but quality of the conference which is at par with any national level conference, that too at such short notice. He further said that this meeting is the only such conference outside the headquarters of TSI, and will act as a precursor to the Annual Conference of TSI at J&K in future. He congratulated the team and appreciated the efforts of organizers, dignitaries, guests and SKIMS administration. Regarding Telemedicine at J&K, he emphasized the need for champions for utilizing the Telemedicine system and leaders making the people make use of the system by the convergence of technology for the implementation of Telemedicine and take forward this technology state-wide. He concluded by advising the audience to leave with good memories and utilize Telemedicine to provide good services to patients.
- Er. Farooq Ahmed Wani, organizing secretary of the event welcomed the guests and thanked Rajiv Rai Bhatnagar and other dignitaries for attending the event. He gave a detailed account of the activities of the Telemedicine Society of India vis a vis Telemedicine services at SKIMS. He said Telemedicine Centre at SKIMS is an essential link in providing the best health care services state-wide and has served as the nerve centre of the JK Telemedicine network, particularly in various disaster situations like the 2005 Earthquake, 2014 Floods and the 2019 Covid 19 Pandemic. He thanked Director SKIMS for supporting and facilitating the event.
- Mr Vimal Vakhloo former president of TSI also spoke on the occasion and Er. Parvaiz A Bhat co-organizing chairman and Chief Engineer SKIMS were also present at the event.
PROGRAMME
The event had a total of 10 sessions of one hour each, spanned over 2 days (5 each day) where each session had 3 slots for presentation or panel discussion. Day first had the first 2 sessions merged and the inauguration session in the afternoon and the day second had a valedictory function at the end. The following is the list of topics for each session.
Besides the usual scientific programme the event focussed on newer emerging digital technologies which are influencing telehealth, strategy besides showcasing the ABDM initiatives.
In the last two decades, the domain has progressed a lot and is still expanding like Artificial Intelligence, Machine learning, imaging informatics, 5G network, cloud, blockchain etc. having potential in healthcare and professional education.
OUTPUT
As evident from the discourse of this conference, the future holds enormous opportunities in the usage of these technologies which are becoming simpler and less expensive day by day and many of them are patient-centric applications in home settings.
The COVID-19 pandemic demonstrated the potential telemedicine offers in augmenting health systems capacity in the UT. During the pandemic, there were operational challenges at multiple levels and there was an urgent need to find the right solutions for contactless healthcare delivery where SKIMS has efficiently used its telemedicine resources to the full extent by using Telemedicine and virtual meetings as the crucial link between all the stakeholders in tackling the pandemic.
Following the outbreak of COVID-19, India’s government has launched new telemedicine guidelines to help healthcare professionals and the ICT industry provide medical services to the population during the lockdown. Even as the health systems transformation envisaged through establishing primary care networks and health and wellness centres under Ayushman Bharat are being established, the Telemedicine Guidelines 2020 provide the opportunity to leapfrog and invert the healthcare delivery paradigm.
Large-scale telemedicine practice in UT would also facilitate the adoption of electronic health records and thereby realize the grand vision for the digital health backbone as envisaged in the National Digital Health Blueprint and strategies outlined by Niti Aayog in Health Systems for a New India: Building Blocks—Potential Pathways to Reforms.
In Summary
As with all technological innovations, telemedicine will be as best at the hands of human experts who leverage it to their advantage. It would be paramount that the health professionals at SKIMS leverage telemedicine to their competitive advantage.
In the long term, empowering citizens, and enhancing user experience in healthcare delivery are likely to improve health-seeking behaviour.
It is high time that digitalisation, cloud solutions, and analytics technologies are leveraged in the healthcare setting, especially at SKIMS. Digitally connected processes enable paperless operations. It is high time for a perception change of viewing IT as an enabler of healthcare delivery.
Further, the process of health planning needs to evolve through the use of Telemedicine in healthcare delivery and distribution and public health decision-making at every level.



AI for Radiology Being Used in Russia
Ms. Filippova Anna
Diagnostics and Telemedicine Center, Moscow Health Department.
Smart algorithms aids doctors in 15 research areas. Now neural networks determine the signs of arthrosis in the knee joint on x-rays and emphysema on computed tomography. This was announced by Ilya Tyrov, Deputy Head of the Moscow Health Department.
“Thus, smart algorithms help doctors in 15 research areas. In total, it already has processed more than 7 million x-rays studies. Further, we intend to expand the application of AI to 29 different areas.” he said.
AI simplifies and speeds up the work of a doctor. It detects and reports even minor deviations and report about it. The doctor receives a picture already marked by the algorithm and describes it independently.
“The radiologist may disagree with artificial intelligence and make a decision himself. The use of such services is not intended to be a substitute for the work of a specialist. You can draw an analogy between modern dictionaries and old ones. You had to open the dictionary and spend a lot of time looking for the right words, now you just need to click on the right link,” said Yuri Vasilyev, Chief Freelance Advisor for Radiation and Instrumental Diagnostics of the Moscow Healthcare Department, CEO of the Center for Diagnostics and Telemedicine.
Nowadays, thanks to smart assistants, it has become less demanding for radiologists to find signs of lung cancer, COVID-19, spinal osteoporosis, thoracic aortic aneurysm, coronary heart disease, stroke, pulmonary hypertension, hydrothorax, as well as lung pathologies, breast cancer and flat feet on CT scans. Neural networks have been introduced into the work of Moscow institutions, which recognize symptoms of 7 different pathologies in one medical image of an X-ray examination at once.
An experiment on the introduction of computer vision into medicine was launched jointly by the Moscow Social Development Complex and the Department of Information Technologies on the basis of the Center for Diagnostics and Telemedicine. Since the start of the Experiment, AI services have processed over 7 million studies. The Center has become a platform for the development of artificial intelligence technologies in Russia, as well as support for domestic developers.
Briefly on the Diagnostics and Telemedicine Center: Diagnostics and Telemedicine Center was established in 1996. It is a top scientific and telemedicine organization under the Moscow Health Department. It specializes in AI implementation in medicine, researches radiation diagnostics, manages departments in medical organizations, including the telemedicine approach.

 TELE ICU – Challenges and Solutions
TELE ICU – Challenges and Solutions
Dr. Raj Raval
President of Telemedicine Of India – Gujarat Chapter
The Indian healthcare industry is under severe pressure owing to a large population and a massive shortage of skilled healthcare professionals including doctors, nurses and intensivist.
- There is a shortage of intensivist in India, and the demand for them is only going to increase with the aging population.
- India will have 5,00,000 ICU beds by 2023, but only 8,350 critical care specialists / Intensivist to monitor it
- Need 50,000 Critical Care Specialists but has just 8,350, As per, the Indian Medical Association source.
- Having timely access to critical care doctors, medical facilities and treatment centers is limited to only a small portion living in developed metro cities leaving a large part of the population living in rural areas without access to quality healthcare.
- Lack of protocols driven ICU.
- High Mortality Rate in ICUs.
- Lack of real time interventions to treat patients.
How Tele-ICU Works
TeleICU is an advanced intensive care solution powered by revolutionary technologies that aim to offer round-the-clock critical care even in the remotest corners of the country.
TeleICU solutions allow hospitals to become robust in early interventions for critical care patients even when they lack professional resources like critical care specialists on-site. Through a multi-pronged, technology-driven approach, Entel Healthtech looks forward to providing best-in-class intensive care facilities to patients requiring advanced level care.
• Entel Healthtech is a technology-driven organization which aims at revolutionizing the existing healthcare infrastructure in the country. Founded by an expert team of medical specialists and technology veterans, Entel Healthtech looks forward to providing high-quality critical care to patients even in the remotest corners of the country, round the clock.
• Using advanced Artificial Intelligence tools and robust technologies, Entel Healthtech aims to solve India’s problem of lack of critical resources in the field of healthcare.
• An expert team of tele-intensivists keeps an eye on patient’s health and vitals using 24×7 tele-coverage feed acquired by the mobile kiosk. Along with real-time feed, they access the patient’s health records and information on on-going treatment.
Direct benefits for a Hospital & Patient through tele-icu
- 1/3rd Cost Saved through TeleICU Services
- Shorter length of Stay for ICU patients
- Lesser Mortality rates
- 24X7 remote monitoring “Crisis Prevention over Crisis Intervention”
- Implementation of International Critical care best
- Digitising ICU Data
- Improving the quality and clinical output
- Acts as an extra pair of Eyes & Ears in the Hospital ICU
- Capacity Building of Bed Side Staff
Entel Healthtech has implemented Tele-ICU located at Godhara, Mahisagar district. The unit established in November 2021.
Saving Life Remotely
A 47- year old female patient, was admitted to General hospital Godhra on December 07 2021. On admission patients have symptoms like tachycardia, Breathlessness,. patient had known case of HTN/ DM .Patient have no any other previous medical history. And vitals are, BP- 190/109 mm hg, pulse- 125, Temp- normal.
Using technology developed and set up at a remote ICU, Team of Experience Critical Care Specialist at Entel Healthtech’s Command Centre clinically examined the patient thoroughly and showed stability in all vitals parameters. During this period of time necessary Reports like Blood investigation + ECG + Chest x ray + ABG had been done.
In this examination there was an abnormality found in ECG and ABG(Compensated respiratory acidosis ). CXR shows pulmonary congestion. By this way Patient was diagnosed with Acute congestive cardiac failure/COPD.
The TeleICU platform used to consult with the primary consultant and patient’s relatives about the future treatment and course of action.It was decided to give medication that can help to reduce chest congestion, control blood pressure and decrease breathlessness.
Throughout the observation and treatment period,Regular discussions were done with the primary consultant about regular reports and medication via TeleICU platform.The patient’s condition improved and he is getting better by each passing day.
These success stories will go a long way in accepting remote monitoring for critically ill patients.

Interesting Telemedicine Research Studies
a.Impact of Telemedicine on Prenatal counseling
The transition from an in-person consultation to a tele-consultation has been significant since the pandemic due to COVID-19. Expecting mothers with a pregnancy complicated by a fetal surgical anomaly were studied before using tele-consultation and after using tele-consultation by a team of researchers. A Mixed method study was performed on the expectant mothers, where both qualitative and quantitative data were analyzed. To know more, please click the link below.
https://www.sciencedirect.com/science/article/abs/pii/S002248042200470X
b.Exploring mHealth potential to improve kidney function: secondary analysis of a randomized trial of diabetes self-care in diverse adults
Individuals living with Chronic Kidney Disease (CKD) are likely to have comorbid Type 2 diabetes. A team of researchers used Telemedicine intervention to reduce the glycemic index in the patient and studied whether it reduced the progression of CKD. The telemedicine support intervention emphasized medication adherence, diet and exercise which significantly improved the individual’s glycemic index. The details of the study can be found by clicking the link below.
https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-022-02885-6
Telemedicine – News from India & Abroad
Your Smartphone can Now Measure Blood Oxygen Levels: Here’s How?
No need to search for pulse oximeters. Your own smartphone camera and flash can now help measure blood oxygen levels easily at home, suggests a new study…..Readmore
Can AI-Powered Robots Laugh at Human Jokes?
Artificial intelligence-powered robot Erica is now trained to laugh at human jokes. Since at least the time of inquiring minds like Plato philosophers and scientists have puzzled...Readmore
Artificial Intelligence Shows Promise in Tuberculosis Detection
An artificial intelligence (AI) system developed could help detect tuberculosis (TB) in chest X-rays at a level comparable to radiologists resources.TB is an infectious disease ….Readmore
Telehealth Linked to Reduced Opioid Overdose Risk?
During the pandemic, the extended use of telehealth for opioid use disorder is linked to decreased risk of overdose, revealed a new study.Published today in JAMA Psychiatry, this study was ….Readmore
Click here to Become a Member of Telemedicine Society of India
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
|
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net





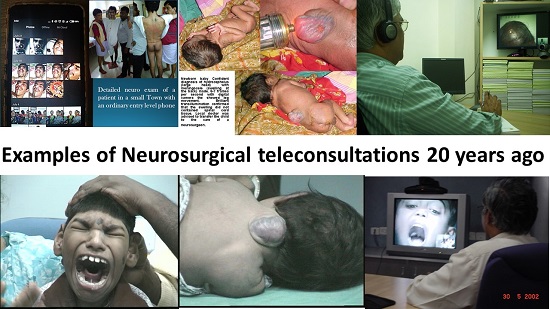
 Teleconsultations between doctors
Teleconsultations between doctors Necessity for formally dually trained Clinician Scientists and Clinician Technologists
Necessity for formally dually trained Clinician Scientists and Clinician Technologists

 Mobile Teladoc Health Robots at MMHRC
Mobile Teladoc Health Robots at MMHRC









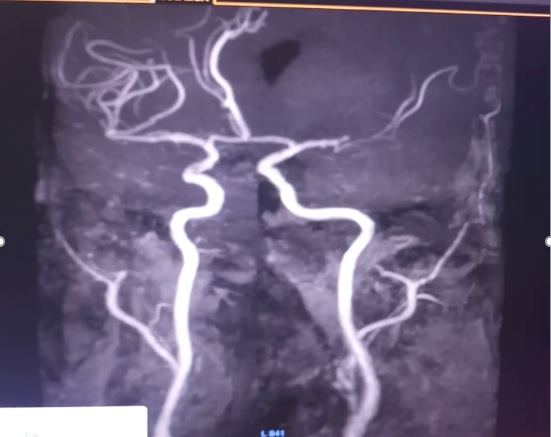
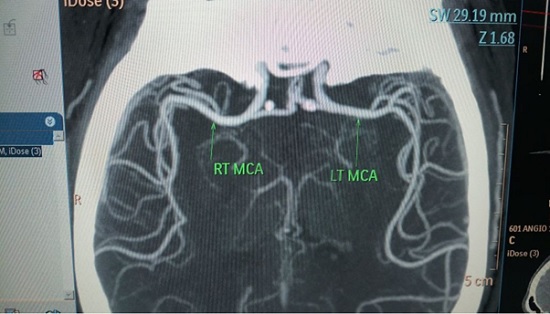
 Role of Telemedicine in Stroke
Role of Telemedicine in Stroke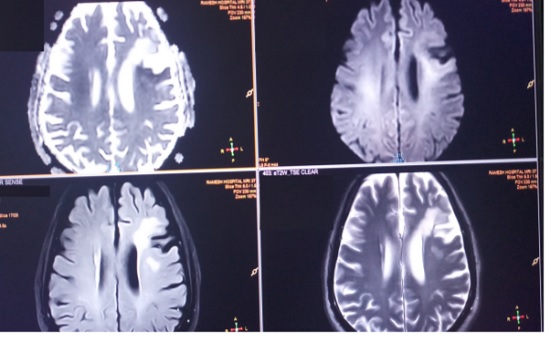
 Tele-Neurorehabilitation: A story from Mumbai
Tele-Neurorehabilitation: A story from Mumbai
 Understanding the implementation of telepractice in speech and language services for children and adults using a mixed-methods approach
Understanding the implementation of telepractice in speech and language services for children and adults using a mixed-methods approach

 Decoding the Healthcare Professional Registry’s Utility in Telemedicine
Decoding the Healthcare Professional Registry’s Utility in Telemedicine TELEMEDICINE IN INDIA: A CRITICAL ANALYSIS OF THE EXISTING LEGAL FRAMEWORK – A Summary
TELEMEDICINE IN INDIA: A CRITICAL ANALYSIS OF THE EXISTING LEGAL FRAMEWORK – A Summary
 Prescriptions and Digital Signatures
Prescriptions and Digital Signatures

 Technology Transformation of Critical Care
Technology Transformation of Critical Care

 eACCESS : Surfing the stormy waves of the pandemic
eACCESS : Surfing the stormy waves of the pandemic
 HTIC HEALTHCARE CONCLAVE – TELEMEDICINE
HTIC HEALTHCARE CONCLAVE – TELEMEDICINE









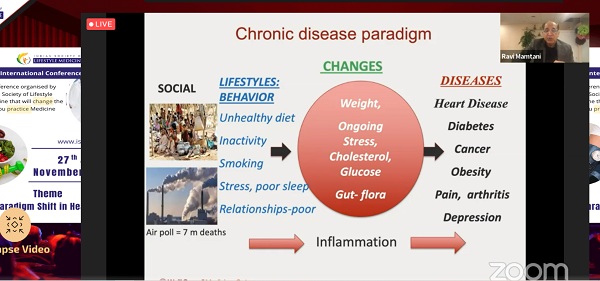
 ‘A Paradigm Shift in Healthcare’ theme of the Second annual conference of Indian Society of Lifestyle Medicine
‘A Paradigm Shift in Healthcare’ theme of the Second annual conference of Indian Society of Lifestyle Medicine