Click Here to Download PDF Version
Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
|
What is New? This issue covers important topics related to Tele-Neurology. We are hoping to bring such focussed newsletters from time to time. This month also saw submission of draft guidelines of the National Medical Commission and includes some of the many recommendations sent to the apex body. These guidelines would have an impact on over a million medical practitioners of the country. Ms. Bagmishika Puhan our health technology lawyer with many others have submitted a document to NMC and so has TSI national body. Thank You |
National Medical Commission, Registered Medical Practitioner (Professional Conduct) Regulations, 2022- Recommendations to the Draft Guidelines
Bagmisikha Puhan
Dr Sunil Shroff
Wing Cdr (Dr) Lavanian Dorairaj (Retd)
Col (Dr) Ashvini Goel (Retd)
Mayank Agarwal
An extensive review and multiple discussions have resulted in the following suggestions for implementation in the draft National Medical Commission, Registered Medical Practitioner (Professional Conduct) Regulations, 2022
Guideline 11 – Guidelines for Practice of Telemedicine in India: Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine.
1. Under Scope at 1.2 – it is necessary to convey it to the practitioners that the exclusions are only rendering them to be outside the scope and applicability of these Guidelines and are not illegal in practice or otherwise. There is a lot of incongruity amongst the minds of the practitioners, with respect to cross-border consultations (during international holidays), standards and interoperability.
2. Under 1.4 – discussing Telemedicine Applications, there is reference to “emergency consult for immediate assistance or first aid etc.” – this should be amended to state emergency consult for immediate assistance, life-saving measures, first aid only with advice for immediate in-person consult or ER visit as available locally.
3. Under 3.2- Identification of the RMP and patient is mandatory – there is a requirement that RMPs should begin consultation by introducing themselves, with mandatory details – there is no clarification provided with respect to consultation in continuity of an in-person consultation/ follow-up consultation; this requirement should not be applicable in such situations.
4. Under 3.4, there is a mandatory requirement to have patient consent which has been further segmented into implied and explicit – depending on who initiates telemedicine consultation. It is imperative that this cannot be the case because tied to the telemedicine consult is the process of seeking personal and sensitive personal information of the patient and the applicable information technology laws mandate that the explicit prior written consent of an individual is acquired, prior to the collection and processing of any sensitive personal data so shared. Hence, while implicit consultation may be acceptable for initiation of a telemedicine consult, there is a requirement to process explicit consent prior to processing of sensitive personal information.
5. Prescription Template – There is a template provided within the proposed Guidelines which was also the same in the earlier iteration. It has requirements to the tune of having details about “provisional/appropriate diagnosis”, “LMP”, “special instructions”, “Investigations”, “Lab Findings”, “Chief Complaints” provided within the prescription.
a. While we agree that these parameters must be captured by the RMP, it is important to note that in the online set-up this prescription is also enabled to be shared with a pharmacy. Without any appropriate privacy laws in place, allowing such details to be shared ahead would not just trigger privacy concerns, but may also cause social stigma attached to medical conditions related to STDs/ VDs, Psychiatry-related, MTP, communicable diseases. Furthermore, it is not necessary for the pharmacist to review and retain information related to the “provisional/appropriate diagnosis”, “LMP”, “special instructions”, “Investigations”, “Lab Findings”, “Chief Complaints” – they need the seal, appropriate prescription made out, and the necessary details of the RMP for dispensation. This excessive sharing is in violation of the privacy of the individual, which has been recognized as a fundamental right by the apex court of the country in Justice KS Puttaswamy (Retd) v. Union of India.
b. It is noteworthy that these details can be retained by the pharmacy, and may be used for data analysis, which is not envisaged by the RMP or the patient and will amount to a strict violation of the privacy principles.
c. At pt. 9, there is a requirement that identification and contact details of the patient must also be added to the prescription – this is again inconsistent with the requirement, purpose of a prescription. This is also excessive in nature and is not in conformity with the template at Annexure 2.
d. There must be stress on digital signatures/ electronic signatures (including AdobeSign, DocuSign, etc.) to ensure that the prescriptions are properly time-stamped and are valid. In absence of this, where scanned files or images of signatures are used by the RMPs to issue a prescription – there could be abuse of this by online pharmacies, or the users themselves, to create / issue new prescriptions for seeking drugs.
e. There is also a requirement under pt. 9, that the e-prescription be valid for a period of 2 weeks from the date of issue or once a pharmacist dispenses the prescribed medications – this might not be a sustainable solution for chronic conditions – and also if a prescription is valid for 2 weeks only, the patient will have to pay further for issuance of another subscription even for a refill for a chronic condition or the likes – this provides platforms with an opportunity to deny treatment or deny dispensation of medication / drugs after a period of 2 weeks.
f. There is a separate template provided under Guideline 2 for writing prescriptions rationally. Similar template should be used for teleconsultations for reconciliation of digitization of electronic/ health records of the patients. The ePrescription for telemedicine consultations has excessive, and confidential data that is not relevant to the pharmacy. It is in fact a case summary and not a prescription. It should be made identical to a standard prescription as mentioned in para-Guidelines 2 Prescription.
6. The Guidelines do not permit technology platforms to indulge in providing ratings, feature testimonials of practitioners on the platform – this will be a hindrance to the users, for the ones who are not familiar with the region / practice of the physician – they tend to rely on these to be able to understand how the particular RMP may address a particular situation, or if they have good bedside manners in dealing with patients. This is indeed a guiding factor to the consumers/ patients of the platform – denying them this right, is impinging upon the users’ right to freedom of speech and expression. While the technology platform may be required to substantiate the ratings – to ensure parity with the listing the Guidelines should not strip this from the platform to enable users make an informed decision in engaging with an RMP for teleconsultation.
7. Under “duties and responsibilities of an RMP in telemedicine”, at para 15, there is a requirement for RMPs to ensure that their medical indemnity cover includes cover for telemedicine – we seek clarification with respect to legislative changes in line with this under professional indemnity and insurance norms.
8. Under “Consultations between RMPs with other RMPs” – there is mention of considering e- ICUs during emergencies like COVID-19 pandemic – remote areas invariably have a specific/ high demand for consultations of this nature. Limiting the prevalence of e-ICUs in cases related to emergencies like pandemics will defeat the purpose of this initiative.
9. Chapter 11 TPG2022 Para 3.5: There needs to be a distinction between a telemedicine consult with a NEW patient for the 1st time as compared to a telemedicine consult with an old patient for a new condition. In the latter case, many if not most details of the patient are already known to the RMP. So, in the latter’s case more Rx flexibility should be allowed.
10. Chapter 11 TPG2022 Para 3.7: Change “If the patient’s condition can effectively and appropriately be managed via telemedicine” to “Once the patient is triaged and the RMP is of the opinion that the condition can effectively and appropriately be managed via telemedicine”.
11. Chapter 11, 1.2. Autonomy and privacy of the RMP: add subpara 9: “The RMP has the right to announce that he/she is terminating the consult (along with the reason) if he/she feels that the same is a crank/prank or abusive call. Details of the same should be recorded to take forward legally, if so desired.”
Guidelines for RMPs and Technology Platforms
12. At 5.5, the onus of ensuring valid registration of the RMP is wholly on the owners and administrators of the technology platform. Owing to lack of continuous online/ physical access to national medical register or respective state medical councils’ registers, several tech platforms are already constrained to avoid onboarding such RMPs whose details cannot be verified by this process causing a loss of opportunity to the RMP and facilitating tech platforms to censure admission of such RMPs. A separate cell/ body should be created to enable platforms to achieve this or seek verifiable information from. There is no set pattern or manner provided to convey if the details of the RMP are legitimate or not; we seek clarification on this specific aspect.
13. At 5.7, tech platforms have been disbarred to counsel patients on the basis of AI and ML, it is pertinent to note that counsel is a wide term and may also include gathering of information from end users, triage of patients, provisioning of general information/ FAQs, which can all be done seamlessly, accurately by these automated tools without disrupting the functioning of the RMP. We are of the opinion that instances like triage, data gathering, or automated responses in form of FAQs be allowed by the usage of AI and ML.
14. At 5.9, its stated that the tech platform may be blacklisted for the violation of TPG by EMRB/ NMC, however, there is no avenue for RMPs to be able to access this publicly – a provision to that effect should be added. Following principles of natural justice, the tech platform should also be provided with opportunity to come back into the ecosystem in the event where this provision is triggered and made applicable to them.
15. It is also important to ensure that there is statement made to the effect that the TPG are technology agnostic and change in technology, mode and media of communication will not impact the compliance that is prescribed and expected under the laws.
In addition to this, our concerns with respect to the initial provisions of the draft guidelines are as below:
16. Chapter 2 Para 4: The prefix of Med Dr is not appropriate as a Doctor of Modern Medicine practices medicine as well as surgery. It would be better to continue to prefix Dr. followed by the full name and prefixed by the qualification. e.g. Dr. Name Family-name MBBS; Dr. Name family-name, MBBS, MS (xxx). The MBBS prefix clearly denotes modern medicine as compared to ayurveda or homeopathy.
17. Chapter 2 Para 4 (E): The RMP should be allowed train, utilize and to provide a certificate of competence to an assistant that he/she has trained under him/her. This would allow increased support in rural areas (especially via telemedicine) while ensuring that the responsibility of ensuring competency of the trained assistants rests with the RMP providing such certifications. This is to bring more clarity to this para with respect to point in chapter 2 para 10 (B) which essentially states the same.
18. Chapter 2 para 8: Suggest “Every RMP is expected to prescribe drugs using generic names” to “Every RMP, as far as possible, must try to prescribe drugs using generic names”.
19. Para 13 D: Suggest “the RMP shall fully digitize records.” To “the RMP shall digitize records.” This is because the efforts to digitize records may not be completed in 3 years.
20. Para 41 (8): An RMP cannot be restricted from practicing in any state. This would affect healthcare adversely especially government, armed forces, etc. doctors who are frequently transferred and who frequently travel to different states for short periods on temporary duty. It would also affect specialists who travel to different cities to provide specialist care to needy patients. Once a doctor is certified and registered in one state he should continue to be allowed to practice all over India as per need. He may, if he so desires, move to register in another state.
21. Chapter 10 CPD: No mention has been given as the age limit for mandatory CPD for registration license renewal. It is generally exempt for seniors. E.G. in Maharashtra it is 65 years after which a RMP need not CPD points for license renewal. Recommend an age limit of 60 years.
22. Under Chapter 2 concerning professional conduct of RMPs, at 9, there is a prohibition on fee splitting or commission imposed on RMP. In the event where the RMPs engaging with the tech platform, it is but obvious that the tech platform will be entitled to charge a fee towards the portal or services. This shall be a deterrent for the platforms. Also, this provision states that RMPs shall not use online forums for procuring patients – this is in conflict with the intent that may be evinced from an association of an RMP with a tech platform. For the entire ecosystem is premised on the fact that it allows the RMPs to widen their outreach, and also enables patients to identify and locate RMPs of their choice, accessibility and affordability.
23. In terms of prescription where the proposed guidelines expect that only generic names can be mentioned – it is worth considering that when RMPs use brand names, they are taking into consideration any enhanced efficacy in such drugs, affordability of the patient and also any positive feedback received or witnessed in their experience with other patients in consonance with their professional judgment. At times for chronic conditions, patients develop affinity, association with a particular brand over a period of time so prescribed to them; in this context, the substitution of the brand name with the generic name of the drug may erode their confidence in the advice of the RMP.
24. At the point of discussion of “Responsibilities of RMPs to each other”, it should be mentioned that in case of a treating physician and a consulting physician, there is a difference in the standard of care owed by an RMP, as opposed to the duty of care owed by the other. This was not mentioned in the earlier iteration, neither the first draft of the TPG, and this also does not find place here. As the draft regulations have delved deep into how relationships are forged or are perceived in case of ascribing duties and responsibilities, it must also consider commenting on the associated liabilities. Guideline 4 under “Assessment of attributability and the severity thereof” – at 2(9) indicates that the role that the doctor is expected to play will be considered – this could be expanded upon to bring out the specific relationship that exists between the treating and the consulting physicians/ RMPs. This becomes imperative in case of telemedicine consultation referrals, wherein the referred RMP may not have the necessary knowledge, history, comorbidities, with a particular patient, and must invariably rely upon the advice, inputs of the consulting physician.
We hope this is in order. We thank you for providing us with the opportunity to participate in this round of stakeholder consultation. We are willing to provide further information in this regard, should there be a need for the same.
Our group has also consulted several physicians, practitioners and have taken the liberty of providing changes to the draft so circulated, by including our suggestions within such document.
 Teleneurology : Are we there?
Teleneurology : Are we there?
Prof. K. Ganapathy
Past President, Telemedicine Society of India & Neurological Society of India | Hon Distinguished Professor The Tamilnadu Dr. MGR Medical University | Emeritus Professor, National Academy of Medical Sciences | Formerly Adjunct Professor IIT Madras & Anna University | Director Apollo Telemedicine Networking Foundation & Apollo Tele Health Services | URL: www.kganapathy.in
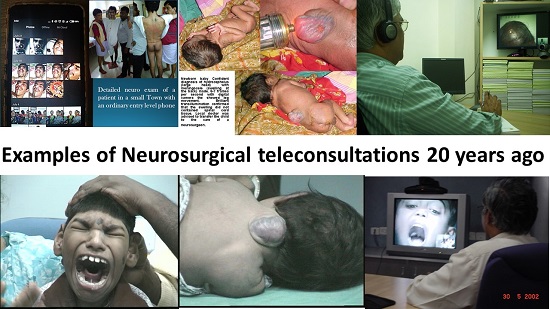
It was in 2015 that the author had pointed out (https://www.neurologyindia.com/text.asp?2015/63/2/142/156274) that there was not a single neurologist or neurosurgeon for a population of 935 million Indians. With 773 districts in India likely to have a medical college, no doubt the urban rural health divide will reduce. However not in the life time of my great grand children will there be an equitable physical distribution of super specialists in India. Of the 675 million internet users (48% penetration) 80% use mobile networks. The slogan today is “ Roti, kapada, makan, and bandwidth” A strand of RNA acting as Global CTO has indeed radically transformed the deployment of telehealth worldwide. The 6000 odd neurologists and neurosurgeons cannot cater to at least 30 million(excluding neuro trauma and neuro infection) requiring their services ref (https://www.neurologyindia.com/text.asp?2014/62/6/588/149365.) Teleneurology is obviously the only solution to extend the reach of the super specialists predominantly located in urban and suburban India. It is gratifying to see that this is slowly being accepted by the consultants and the beneficiaries (DOI: 10.4103/0028-3886.232346)
There have been at least 20 publications in the last three years from India alone dealing with use of Telemedicine in various subspecialties of neurosciences including tele neuropathology (doi:10.4103/0973-029X.1859240 tele neurorehabilitation 10.4103/aian.AIAN_127_21, neuro trauma, (DOI: 10.1016/S0973-0508(04)80019-4, teleneurology during Covid-19 https://www.neurologyindia.com/text.asp?2020/68/3/555/288994 (telestroke (doi: 10.1111/ijs.12326) and Teleneurointensive care ( https://www.neurologyindia.com/text.asp?2021/69/2/245/314591) During the 2nd and 3rd wave many DM, M.Ch and DNB exams in neurosciences were conducted virtually using truly innovative methods https://www.annalsofian.org/text.asp?2020/23/4/429/290022
“Tele” is only a tool to achieve the end, which is making available the “neuro” component available in places where the latter does not exist., “Customer delight” is not a cliché used as marketing ploy. The role of the patient is changing. They are now at the center of self-care becoming a “digitally engaged” patient. Technology acceptance, behavioural modification, increasing digital infrastructure and requirements will cause a paradigm shift in delivery of teleneurology. For teleneurology to succeed the practitioners should strive to produce a “wow” effect. One needs to get into the mind of the end user. Healthcare is personal – it is very hard to feel your experience was excellent, when those treating you do not introduce themselves, or make eye contact, or say what they are doing to you and why. Conversely, when those simple things are addressed, the experience rapidly improves. Achieving excellence in healthcare is neither difficult nor expensive. It does not matter if care is cutting-edge and technologically advanced, if it does not take into account the patient’s goals. In fact it may not even be worth doing. Patients do not care how much the doctor knows. They want to know how much the doctor cares!!
Webside manners is replacing bedside manners of the 20th century. https://www.youtube.com/watch?v=BJYp7Ti8noo. Patient rapport is crucial particularly in neurology. 80% of messages are conveyed non verbally through body posture, voice intonation, the way one looks / sits, attire, movement of hands, arms and spontaneous smiling. The practice of medicine is an art, not a trade, based on science. This must be absorbed in the new science. Health care is a calling not a business.
Innovative methods like Group Telecounselling needs to be deployed. Contrary to a common misconception that doctor patient relationship is strictly confidential and always one to one, studies have revealed that patients are more @ home with other patients having similar problems. With acute shortage of neurologists and neurosurgeons, patients with common clinical conditions can be reviewed remotely in groups in one session eg seizures, post head injury sequelae, migraine etc. This would save time and be cost effective and enable larger numbers to get specialist care.
Distance has become meaningless. Geography has become History! The world will never be the same again. It is imperative that we accept and start deploying the “New Normal”. Technology enabled remote health care in neurosciences is here to stay.
 Role of Telemedicine in Stroke
Role of Telemedicine in Stroke
Veteran Major General Dr. S. Kumaravelu
Professor and Head Neurology, Ramesh Cardiac & Multispeciality Hospitals Pvt Ltd, Guntur
Stroke is the second leading cause of death after Coronary heart disease and the most common cause of disability in adults with huge social and economic burden. Telemedicine has revolutionised the management of stroke. It has a key role in prevention, hyperacute care, follow up and education of stroke. As regards prevention, it has a significant role to play in secondary prevention. We have regular telemedicine consultation for all our stroke patients to ensure proper diet control, and control of risk factors for stroke and ensure physiotherapy, both by a physiotherapist and caregivers.
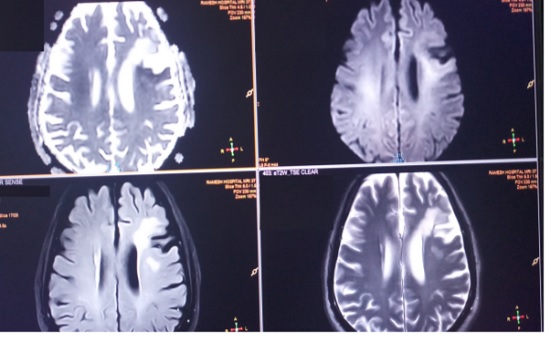
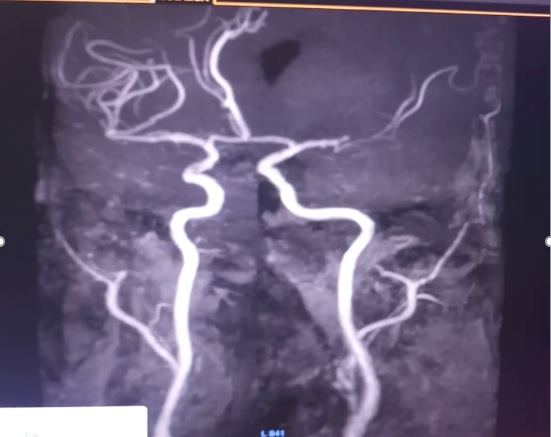
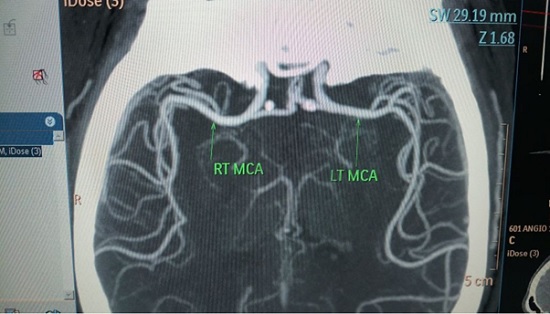
Regarding hyperacute care, I shall narrate a different case scenario. Our patient a middle aged male was brought to our Emergency room at 11: 35 hours with history of sudden onset inability to speak, Confusion and staring look since 10:30 hours. He was a known patient of type 2 Diabetes Mellitus, Hypertension, Coronary artery disease with coronary artery bypass graft done and posterior circulation stroke on medication. He also had peripheral arterial disease as well with embolectomy done earlier. He came within a window period of 65 minutes. His imaging was done. His Magnetic Resonance Images and Angiogram are shown as Fig 1 and 2 respectively. The imaging was completed within 30 minutes. He was diagnosed as a patient acute ischemic stroke left middle cerebral artery territory with left middle cerebral artery occlusion. I, being the only Neurologist was away from the hospital. As the stroke was within 4.5hour window, it was decided to offer thrombolysis to the patient. Real time video consultation was given through a video portal. The family agreed to undergo thrombolysis. The thrombolysis clinical protocol was initiated. The indications and contraindications were enquired into. The severity of stroke was assessed using the NIHSS (National Institute of Heath Stroke Severity). His stroke score was 13. After taking informed assent from the wife, telethrombolysis was initiated with injection Actilyse 7 mg intravenous bolus followed by 63 mg intravenous infusion over the next one hour. Patient showed significant improvement with return of speech, and improving weakness of right half of body. Repeat Computerized Tomography angiogram of brain and neck revealed complete revascularization of the left middle cerebral artery.
Telestroke is an emergency telemedicine application that provides physicians with immediate access to neurologists who can support both the assessment and treatment of patients experiencing acute ischemic stroke symptoms. Using teleradiology to review Computerized Tomography (CT) images and videoconferencing solutions, the off-site neurologist can assess the patient and provide recommendations as to whether patients are candidates for thrombolysis and other interventions for acute stroke. The decision to use the thrombolytic (clot busting) agent tPA (tissue plasminogen activator) requires a Neurologist and the drug must be administered as soon as possible within the 4.5 hours following stroke onset. Telestroke is considered to be a key strategy to achieve equitable access to high quality care for stroke for all people. Without Telestroke, many patients living in and around communities lacking a neurologist would simply be denied the benefit of treatment with thrombolysis, or tPA, which is a best practice standard of care for acute ischemic stroke. This has been justified by the American Stroke association in their guidelines.
1. Telestroke/teleradiology evaluations of AIS patients can be effective for correct IV alteplase eligibility decision making.
2. Administration of IV alteplase guided by telestroke consultation for patients with AIS can be beneficial.
3. Telestroke networks may be reasonable for triaging patients with AIS who may be eligible for interfacility transfer in order to be considered for emergency mechanical thrombectomy.
4. Providing alteplase decision-making support via telephone consultation to community physicians is feasible and safe and may be considered when a hospital has access to neither an in-person stroke team nor a telestroke system.
Hence it may be concluded that Telestroke is the only solution to serve suburban areas and to increase thrombolysis rates.
Coming to the next aspect of telestroke, the most important aspect for advocacy and education regarding stroke is feasible through webinars and videoconferences. Imparting such knowledge will ensure equitable medical care beyond the urban limits to the needy patients in rural areas.
 Tele-Neurorehabilitation: A story from Mumbai
Tele-Neurorehabilitation: A story from Mumbai
Prof. Nirmal Surya
Chairman, Surya Neuro Centre, Mumbai, Associate Professor, Bombay Hospital and Medical Research Centre, Mumbai.
Dr. Guhan Ramamurthy
Consultant Neurologist, Institute of Neurosciences and Neurorehabilitation, BG Hospital, Tiruchendur, Tuticorin.
Tele-Neurorehabilitation:
COVID-19 has ravaged economies, societies and human life across the world, and distanced people. The health care resources were strained and depleted. This had resulted in the inability of health care to cater to other non-COVID health services. With the increasing requirement of health care services, the inadequate reach of services to the needy patients and to make ends meet, the popularity of telemedicine emerged during these difficult times.
Telemedicine provides a platform for the exchange of information between the healthcare professionals, and the patient in arriving at the diagnosis and the management of patients. Telemedicine in Neurology (Tele-neurology) is useful for teleconsultations, tele-neurorehabilitation, and tele-research. The tele-neurology can be performed through mobile or computer-based applications. The Government of India has issued telemedicine guidelines for aiding the practitioners (https://www.mohfw.gov.in/pdf/Telemedicine.pdf). It is a prerequisite to obtain the patient’s consent (guardian’s consent in case of a minor).
Neurorehabilitation was no exception and had initially succumbed to the wrath of the COVID-19. However, the healthcare professionals had coped up with the new normal and adopted tele-neurorehabilitation. We were able to deliver tele-neurorehabilitation to patients with acute neurological deficits and chronic neurological deficits. It was useful to assess the patient’s deficit, formulate and tailor protocols to the requirements and needs of the patient and follow up on their progress. The tele-neurorehabilitation was as efficient as in-person neurorehabilitation in terms of clinical improvement. Further, the tele-neurorehabilitation had helped in providing the expertise in rural areas where it was scarce. The team members involved in tele-neurorehabilitation include a neurologist, physiatrist, physiotherapist, occupational therapist, speech and language pathologist, cognitive psychologist, nurse, social worker, and caregiver.
The story from Mumbai:
The Epilepsy Foundation India is aimed at providing comprehensive care to patients with epilepsy. The comprehensive care includes tele-neurology consultation (HIPAA compliant), pharmacological treatment, tele-neurorehabilitation, and abolishing the misconceptions associated with epilepsy. The needy patients were provided with drugs, free of cost.
The tele-neurorehabilitation session included yoga therapy, cognitive therapy, counselling, occupational therapy, and physical therapy. Yoga therapy was provided as a weekly session to reduce stress and improve seizure control. The clinical psychologist provided weekly counselling sessions for the patients to better handle stress due to the stigma of patients with epilepsy and the burden created by COVID-19. The cognitive therapist provided cognitive training. The caregiver was encouraged to perform 3-5 sessions of cognitive rehabilitation per week. The patients were provided with physical and occupational therapy and were encouraged to continue 2-3 sessions per day for 5 days/week.
The model adopted during times of COVID-19 that warranted social distancing is also useful to deliver expert care to patients in rural areas and ensure continuity of care. The comprehensive care was provided to patients through tele medicine platform and serves as a model in the comprehensive care of epilepsy patients. It can be extrapolated and tailored to the management of other neurological disorders.
The tele-neurorehabilitation is also useful in the rehabilitation of patients with postural imbalance and falls by improving balance, improving motor strength in upper and lower limbs through strength training, cognitive rehabilitation using restorative or compensatory strategies and rehabilitation of patients with multiple sclerosis.
The way forward:
Tele-neurology is cost effective, easy to use. It helps the patient to receive treatment from their home improving their comfort and saving travel time and cost. It also helps to prevent acquiring COVID-19, especially in the vulnerable patients with neurological disorders, who are at increased risk of complications resulting from COVID-19.
However, tele-neurology though it brings the world closer, it lacks the human touch and certain techniques of examinations are difficult to perform. It requires the doctor and the patient to be adept at modern technology and communication. The privacy, and confidentiality of patient data should be vigilantly maintained.
Tele-neurology has emerged during the times of COVID-19 and helped us deliver health care at times when social distancing was the norm. However, it has become an integral part of neurological evaluation and management that it is bound to fortify for the times to come as the COVID-19 fades into thin air. Updates and modifications to the existing guidelines shall be required as the practitioner faces newer challenges in delivering healthcare through tele-neurorehabilitation. The use of virtual reality in telerehabilitation can bring the healthcare professional and the patient together in the same virtual room augmenting the interaction.
Telemedicine – News from India & Abroad
Artificial Intelligence Helps Identify Benign Thyroid Nodules
Artificial intelligence (AI) pinpoints thyroid nodules noticed on thyroid ultrasound that are unlikely to be cancerous. The technology reduces a large number of unnecessary biopsies……Readmore
Simple App May Help Ease Insomnia
Treating insomnia becomes feasible without the use of medications as scientists design a new therapeutic app. Insomnia is a common and debilitating sleep disorder that can impact a person’s physical and mental health and wellbeing….Readmore
Click here to Become a Member of Telemedicine Society of India
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
|
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net


 Teleneurology : Are we there?
Teleneurology : Are we there? Role of Telemedicine in Stroke
Role of Telemedicine in Stroke Tele-Neurorehabilitation: A story from Mumbai
Tele-Neurorehabilitation: A story from Mumbai