
Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
What is New?
This issue features some interesting articles, including one from the Medical Board of Australia discussing the issuance of prescriptions during Telehealth consultations. Another captivating piece titled “Leveraging Emerging Technologies for Healthcare – Smart Health” by our former president Mr. Vimal Wakhlu, delves into employing cutting-edge technologies such as AI, Extended Reality, Blockchain, Big Data Analytics, Quantum Computing, IoT, and 3D Printing to achieve Sustainable Development Goal 3 (SDG-3), which aims to “Ensure healthy lives and promote well-being”. He explores how these technologies can particularly aid India in reducing maternal and infant mortality, as well as combatting communicable and non-communicable diseases.
With AI progressing at a brisk pace, it is imperative to contemplate the fundamental principles and strategies necessary for its regulation in healthcare, to safeguard patient safety without stifling innovation. A concise article sheds light on this topic, pinpointing key considerations and focus areas for regulatory strategies in the healthcare sector.
For those interested in coding, Dr. Sridhar presents an engaging article that guides you through simple steps to get started. Should you encounter any challenges, he’s available for assistance. His infectious zeal may inspire some to begin experimenting and enjoying the process.
Additionally, let’s appreciate that the month of June, named after the Roman goddess Juno. It has brought some respite from heat by the refreshing onset of the rainy season. In fact, for the first time in 62 years the monsoon arrived on the same day both in Delhi and Mumbai.
Thank You
Dr. Sunil Shroff
Chief Editor
President – TN Chapter – TSI
Leveraging Emerging Technologies for Healthcare – Smart Health Part1
Vimal Wakhlu
Good Health and Wellbeing is one of the Sustainable Development Goals(SDGs)- SDG3. SDG-3 of Sustainable Development Goals-SDGs 2030 states- “Ensure healthy lives and promote wellbeing”. The primary objective of SDG3 is to ensure healthy lives and wellbeing for everyone, regardless of age, gender, or socioeconomic status. It aims to address various health challenges, reduce preventable deaths, and promote physical and mental well-being, and in the process envisages:
#1 Reducing maternal mortality and ensuring access to quality maternal and reproductive healthcare services.
#2 Ending preventable deaths of newborns and children under 5 years old, with a focus on tackling major diseases, malnutrition, and providing vaccinations.
#3 Combating major communicable diseases such as HIV/AIDS, malaria, and tuberculosis, as well as non-communicable diseases like cancer and cardiovascular diseases.
#4 Ensuring universal access to healthcare services, including access to essential medicines and vaccines, and strengthening health systems.
#5 Addressing substance abuse, promoting mental health, and providing access to affordable and quality healthcare services for all.
Emerging Technologies like Artificial Intelligence, Extended Reality, Blockchain, Big Data Analytics, Quantum Computing, Internet of Medical Things,3D Printing, Digital Twins, Drones etc. ensure that concepts like Digital Health can be implemented to leap frog the traditional approach, as there is an acute shortage of all resources, including trained health professionals at the global level.
Artificial Intelligence (AI) and data analytics: Healthcare data, including maternal health records can be analyzed, to identify patterns and risk factors associated with maternal mortality and complications, since it varies from place to place. These technologies can help develop predictive models to identify high-risk pregnancies, provide personalized care plans, proactive intervention. (#1)
AI can help analyze disease patterns and environmental factors, to detect outbreaks and anticipate disease trends. Early detection and response to outbreaks can prevent the spread of infectious diseases and enable targeted interventions to protect children’s health. (#2)
AI can also analyze, genetic information and molecular structures, to accelerate drug discovery and development. It can also identify potential drug candidates, optimize treatment regimens, and predict drug responses. This can significantly impact the development of new therapies for communicable and non-communicable diseases, including HIV/AIDS, malaria, cancer, and cardiovascular diseases. (#3).
Data analytics and AI algorithms can also analyze large-scale healthcare data, providing insights for evidence-based decision-making and resource allocation. These technologies can help optimize healthcare delivery. It can also support clinical decision making, risk stratification, and personalized treatment plans, improving health outcomes and efficiency of care. (#4)
Data from online assessments, surveys, and social media can be analyzed to identify individuals at risk of substance abuse or mental health disorders. It can assist in the early identification of symptoms, prompt appropriate interventions, and guide personalized treatment plans. It can also improve the efficiency of mental health screenings and support the scalability of services. (#5)
Telemedicine and telehealth: Prenatal care, postpartum care and advice on reproductive health can be enabled through telemedicine network in rural and remote areas as well. Video consultations, and remote monitoring devices can be helpful in the process. (#1)
Telemedicine platforms can connect healthcare providers with patients in remote guidance, consultations, and follow-up care for both communicable and noncommunicable diseases. (#3)
Telemedicine facilitates access to healthcare services, including primary care, specialist consultations, and follow-up visits. It can reduce travel costs and time, overcome geographical barriers, and improve healthcare access for marginalized populations. (#4)
Teletherapy and online counseling services enable individuals to receive therapy, counseling, and support for substance abuse, addiction, and mental health issues. Teletherapy thus expands access to mental healthcare, especially for those in underserved areas or facing barriers to in-person services.(#5)
Electronic Health Records (EHRs): EHRs can help improve the management of maternal healthcare information in terms of a comprehensive and centralized record of a woman’s medical history, facilitating continuity of care between different healthcare providers, thus leading to informed decision-making, reduced medical errors, and improved coordination during the course of this entire cycle.(#1).
EHRs for children can help in the comprehensive management of vaccination records, growth charts, and medical history, besides improving coordination of care, and enable healthcare providers to identify trends, patterns, and gaps in healthcare delivery. (#2).
EHRs and data analytics can facilitate comprehensive management of patient information, disease surveillance, and research, besides enabling tracking of disease trends, identifying risk factors, and developing targeted interventions for communicable and non-communicable diseases. Data-driven insights can help formulate public health strategies, personalized treatments, and early interventions.(#3)
EHR systems can streamline healthcare delivery, improve coordination of care, enhanced patient safety, besides enabling healthcare providers to access patient information and medical history, reducing duplication of tests, improving medication management, and supporting continuity of care. Also this process can contribute to data collection for health system monitoring, resource allocation, and policy planning. (#4)
(To be continued)
[This article has been first published in Communications Today in June 2023 as
Healthcare 2.0: Unlocking Opportunities with Emerging Technologies]

Healthcare’s Digital Custodians: Steering the Course of AI Regulation for a Safer Tomorrow
Dr. Sunil Shroff
President, Tamil Nadu Telemedicine Society of India | Consultant Urologist & Transplant Surgeon
The advent of Artificial Intelligence (AI) has revolutionized the healthcare industry. Within a short span we now have available predictive analytics using patient data to robotic surgeries. However, alongside the benefits, there are challenges and risks that need to be immediately addressed. The challenge is to determine what are the essential principles and strategies for regulating AI in healthcare to ensure patient safety without inhibiting innovation and development.
AI in healthcare encompasses various applications that include – diagnostic tools, treatment planning, drug discovery, and patient monitoring. These applications can improve healthcare delivery and add tremendous value by enhancing accuracy, efficiency, and personalized care. However, the misuse or malfunction of AI systems could have dire consequences and is scary. It can lead to misdiagnosis, privacy violations, and inequitable healthcare services.
Principles and Strategies for Regulation:
1. Patient Safety and Efficacy: Ensuring patient safety is paramount. Regulatory bodies must require that AI systems in healthcare undergo rigorous testing and validation before deployment. In the US it is proposed that the Food and Drug Administration (FDA), for instance, should assess AI systems in terms of both safety and efficacy, ensuring they meet specific standards before approving them for clinical use. In India, even the healthcare apps have so far no regulations or certification.
2. Data Privacy and Security: Healthcare AI systems often rely on patient data, which is sensitive and personal. The regulation must ensure that AI systems comply with data protection laws, such as the Health Insurance Portability and Accountability Act (HIPAA) in the US, ensuring the confidentiality and security of patient data. Patients should have the right to know how their data is being used and to consent to or opt-out of data sharing. Currently in India we still are awaiting the parliamentary approval of the PDP bill.
3. Discriminatory practices Bias and Fairness: AI systems can inherit biases and this can be unintentional as they would be more inclined to provide results from the data they are trained on and this can lead to discriminatory practices. Hence it is critical to enforce regulations that mandate the use of diverse and representative datasets in the development of AI tools. However currently diverse clean datasets may not be available. AI systems should be continuously monitored for biases, and corrective measures should be taken if any disparities are identified.
4. Transparency: AI systems’ decision-making processes should be transparent and interpretable by healthcare professionals. Doctors must understand how an AI system arrived at a particular diagnosis or recommendation. This aids in fostering trust among healthcare providers and ensures that AI acts as a decision-support tool rather than a decision-maker. For this to be effective doctors would require some training into how AI decision-making processes works.
5. Liability and Accountability: Clearly defining liability in case of AI failures or errors is essential. Regulations must determine who will be held accountable – the AI developers, the healthcare institution, or the individual practitioners. Clear accountability structures can ensure prompt responses to issues and reinforce the responsible deployment of AI in healthcare. This regulations would to an extent also apply for privacy and confidentiality issues, hence could be addressed within the PDI bill or in the IT act.
6. Human Oversight: AI should complement, not replace, human expertise in healthcare. Regulations should mandate the presence of human oversight bodies, particularly in critical decision-making areas. Doctors and medical professionals should have the final say in patient diagnoses and treatments, ensuring that AI recommendations are validated through human judgment. This has been incorporated in the Telemedicine Practice Guidelines from the Ministry of Health.
7. Continuous Monitoring and Post-Market Surveillance: AI systems in healthcare must be subject to ongoing monitoring and post-market surveillance to ensure that they continue to perform safely and effectively in real-world settings. Just like for drugs regulatory frameworks must facilitate the reporting of adverse events and allow for the recall or modification of AI systems that do not meet safety or efficacy standards.
8. Global Collaboration and Harmonization: AI in healthcare is not constrained by borders. International collaboration is essential for sharing best practices and harmonizing regulatory standards. Global organizations, such as the World Health Organization (WHO), can play a significant role in facilitating international dialogue and cooperation on AI regulations in healthcare.
The integration of AI into healthcare holds tremendous promise for improving patient outcomes and healthcare delivery. However, this must be balanced with comprehensive regulations that prioritize patient safety, data privacy, fairness, transparency, human oversight, continuous monitoring, and accountability.
Through thoughtful regulation and global collaboration, we can harness the power of AI applications in healthcare and safeguard all the stakeholders.

Coding for fun
Dr. Bodapati Sridhar
Founder and CEO, EdQueries LLP
All of us use software these days. Software is made by writing code and creating stuff and watching others use it is fun. Just like poets enjoy writing poetry and want everyone to hear their poetry. In case you are wondering which coding I am referring to; it is the code used in Software programming; not the codes used in Electronic Medical Records.
But for many it’s a daunting task. Therefore, in this article and a few following ones, I will attempt to make it simple, and fun.
To get started, let’s download Visual Studio Community edition (it’s free!), by clicking this link. You can download it for your Windows laptop or PC as well as for Apple’s Mac. Visual Studio is a very powerful tool and makes coding extremely easy.
To begin with, we will be creating some very simple Console applications. Console is the black screen on which you enter commands. It’s not frequently used these days, but it makes life easy for beginners learning to code for the first time.
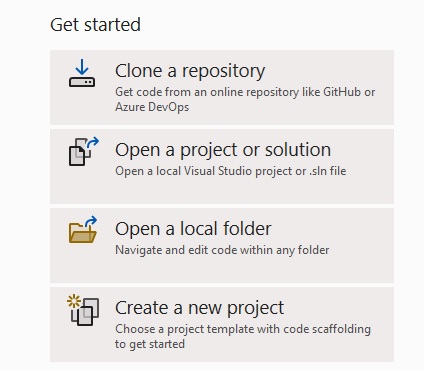
Once you have downloaded Visual Studio Community edition, click the “Create a new project” button.
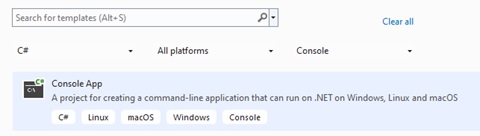
Then, select C# Console App (you can use the Search box to get it)
Click the ‘Next button’ and then give your project a name.
Usually, the first project someone makes is called “Hello World”. It’s a nice convention you may want to follow.
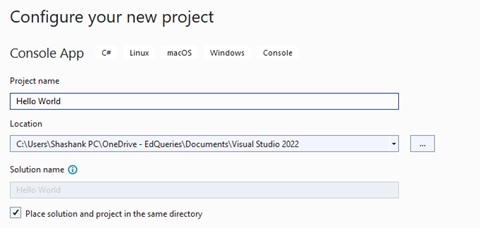
Click ‘Next’ again and finally click the ‘Create’ button.
You should now see something like this:
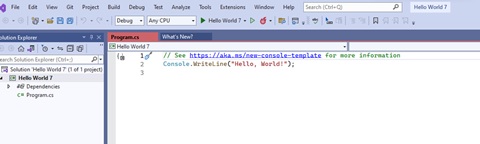
This statement will write the message specified in double quotes on the Console : Console.WriteLine(“Hello World”)
Click the “Play “ button on tool bar ( the button to the left of the ‘flame’ icon in the image below).
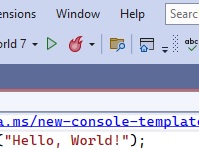
A black screen should load in a moment, with “Hello World “written.

Now, let’s close this black window (this is the ‘Console’).
It’s time we changed the message displayed on the ‘Console’. Close the ‘Console’. Now, in Visual Studio, write your name, instead of “World”; say hello to yourself. I wrote “Hello Sridhar” and clicked the ‘Play’ button again.
Now, the ‘Console’ shows “Hello Sridhar”.
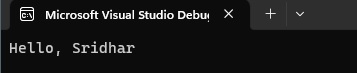
We have successfully written a message to the ‘Console’.
Now, let’s write other messages. Write Console.WriteLine(). Inside the two round brackets, insert double quotes and write some text. Do this three times by writing three different messages using Console.WriteLine(). Each time, you must end the line with a semi-colon. The semi-colon tells your computer that the line of code is complete.
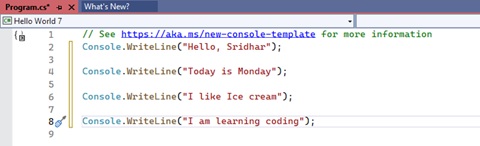
After writing these messages, click the ‘Play’ button again.
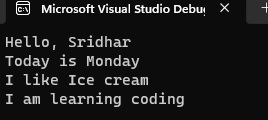
If you have successfully displayed more messages on the ‘Console’, then you have written lines of code to display output on the ‘Console’. Congratulations!
We have taken our first baby steps into the world of Software programming.
The words or sentence inside the double quotes can be stored elsewhere, so that the line of code can be re-used multiple times. That storage space we will create is called a ‘Variable’; and if we are storing words or sentences in it, it’s called a ‘string’ type of variable. ‘Variables’ can be of various types. E.g., ‘string’ stores words or sentences while a variable of type ‘int’ stores numbers (‘int’ represents Integers).
Well, let’s try them out.
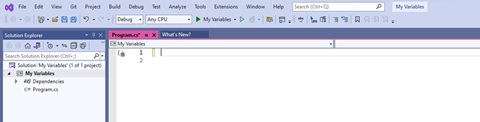
Let’s start afresh. Create a new project by following the above steps. Give a name to the new project e.g. My Variables
This time delete everything that’ pre-written for you, including the “Hello World” statement.
You should have an empty central area in Visual Studio, like this:
Now, create a “variable of type “’string’ “like this.
string s = “Ice cream”;
Since we are creating a variable of type ‘string’, we must enclose the words or sentence after the = sign in double quotes. After that end the statement with a semi-colon.
Now, you have stored the words inside a ‘variable’ . You have also given a name to the variable. I have name it “s”. But I could have named it anything else. E.g. I could have named it “myFirstVariable”. The code would then look like this:
string myFirstVariable = “Ice cream”;
The ‘variable’, as mentioned above is a storage space. You have given the storage space a name so that you can call it by that name whenever you need it. You have then stored some text inside that storage space. Now, let’s use our variable, by writing this code:
Console.WriteLine(s);
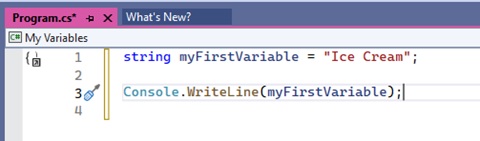
Now, “Play” this code.
You should see your text in the Console window.
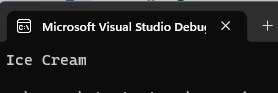
Now, let’s change the text we stored in the variable, like this:
‘string’ myFirstVariable = “This is what I want to do today”;
Now, play it again. The Console will display the new text, because you changed what is stored in the variable.
If you have tried all the above steps and successfully displayed messages on the Console, you have taken your first steps into the world of coding.
The language we are used is called “C Sharp”, written as “C #” also. There are various programming languages out there, each with a specific purpose. I have chosen this one, because it comes from Microsoft and it can be used for creating desktop applications, mobile applications, websites, video games and various other types of software. Also, because of Visual Studio and it’s built in “IntelliSense, it’s quite easy to learn.
Common causes of errors: In C-Sharp, capital letters and small letters are considered different things. “String” and “string” are not the same. If you have named the variable as “MyFirstVariable”, but elsewhere in your code, you called it “Myfirstvariable”, then your code won’t work, as you changed capital letters and small letters changed.
Another common source of errors is the semi-colon. Don’t forget to add a semi-colon at the end of each statement.
That’s all for now. As you try out more coding, you will start enjoying it. Try it today. Try writing various other sentences. Create more variables. Keep coding.
(If you get stuck during coding and require help, you can call Dr. Sridhar at 94490 58818. It may be best to send him a message first)
New Telehealth Guidelines issues by Medical Board of Australia for Prescriptions
Updated telehealth guidelines will close the gap that’s sprung up between online prescribing business models and good medical practice.
After consulting the community and profession, the Medical Board of Australia has today issued revised telehealth guidelines that will take effect on 1st September 2023.
Under the updated guidelines:
Telehealth consultations will continue as an important feature of healthcare in Australia.
Real-time doctor-patient consultations remain key to safe prescribing.
Prescribing via questionnaire-based asynchronous web-based tools in the absence of a real-time patient-doctor consultation is not considered good practice.
‘Telehealth is here to stay. It plays an important role in healthcare in Australia and has opened great opportunities to improve access to and delivery of care, including to rural and remote patients and people living with disadvantage,’ Board Chair, Dr Anne Tonkin AO said.
The interaction between a doctor and their patient is an important element in all consultations, including telehealth consultations.’
The standard of care provided in a telehealth consultation must be safe and as far as possible meet the same standards of care as provided in an in-person consultation.
But prescribing or providing healthcare for a patient without a real-time direct consultation, whether in-person, via video or telephone, is not good practice and is not supported by the Board.
The guidelines specify that:
‘This includes asynchronous requests for medication communicated by text, email, live-chat or online that do not take place in the context of a real-time continuous consultation and are based on the patient completing a health questionnaire, when the practitioner has never spoken with the patient.
‘Any practitioner who prescribes for patients in these circumstances must be able to explain how the prescribing and the management of the patient was appropriate and necessary in the circumstances.’
‘A doctor who has not consulted directly with the patient and does not have access to their medical records is unable to exercise good, safe clinical judgement,’ Dr Tonkin said.
Under the guidelines, a patient’s usual medical practitioner, or another health practitioner with access to the patient’s clinical record, can prescribe without a consultation in certain circumstances.
The guidelines allow a patient to consult a doctor for the first time using telehealth and for a doctor to issue new and repeat scripts as part of a telehealth consultation. The Board does not expect a patient to have had an in-person appointment with a doctor before they have a telehealth appointment.
‘Prescribing medication is not a tick and flick exercise. It relies on a doctor’s skill and judgement, having consulted a patient, and recognises that prescription medication can cause harm when not used properly,’ Dr Tonkin said.
The Board carefully considered the feedback from customers of asynchronous prescribing companies who argued that their programs were convenient, including when they couldn’t get GP appointments.
‘But prescribing medication should not occur in isolation,’ Dr Tonkin said.
‘Consultations enable a doctor to ask follow-up questions that help identify the best treatment for a patient, including when they have previously been given a script by another doctor,’ she said.
President Professor Steve Robson of the Australian Medical Association said the MBA revision of the guidelines was necessary to build a sound foundation for telehealth now and into the future.
“The rapid growth of telehealth in recent years spurred on by the Covid-19 pandemic means it is important doctors have clear guidance on its use.
“The guidelines strike the right balance by ensuring telehealth remains accessible for patients, while at the same time discouraging poor models of care that can result in missed or misdiagnosis.
“Telehealth should be seen as an additional tool to assist doctors to provide good medical care to their patients. It should be used to augment and build on the care provided by a traditional face-to-face consultation.
“The guidelines note that while best practice use of telehealth is in the context of a continuing clinical relationship, there are other circumstances where it will be appropriate.
“They also make clear that prescribing in the absence of a real-time patient–doctor consultation for patients with no existing relationship is not appropriate and rarely acceptable.”
One can access these guidelines – https://www.medicalboard.gov.au/Codes-Guidelines-Policies/Telehealth-consultations-with-patients.aspx

Telemedicine – News from India & Abroad
How Does ChatGPT Help Physicians You Pick the Right Imaging Tests?
ChatGPT was found to support the process of clinical decision-making, including when selecting the right radiological imaging tests for Breast cancer screening…. Readmore
How Artificial Intelligence Can Help Predict Cybersickness in VR Users
With the growing use and need of VR technology, being able to effectively predict and prevent cybersickness was crucial, said researchers from Charles Darwin University (CDU) and Torrens University in Australia…..Readmore
Precision in the Future of Medicine Achieved by AI Program
Developed by researchers at NYU Grossman School of Medicine, an AI program analyzes physicians’ notes to accurately predict patients’ risk of death, length of hospital stay, and other crucial care factors…Reademore
The Paradigm Shift Towards AI With Soul
In the modern world, automated systems and artificial intelligence have become essential in our daily lives. However, their pervasive use raises ethical dilemmas for technologists and developers….Readmore
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
- Report can be from 500 to 600 words
- Report Should be relevant to Telemedicine or Medical Informatics
- No promotion of self or any product
- Avoid plagiarism
- All references should be included
- Provide any attributions
- Visuals are welcome including video links
- Send full authors name, degrees, affiliations along with a passport sized photograph of good resolution. If multiple authors only main author photo to be sent.
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net

