Telehealth Newsletter
Official Newsletter of Telemedicine Society of India

What is New?
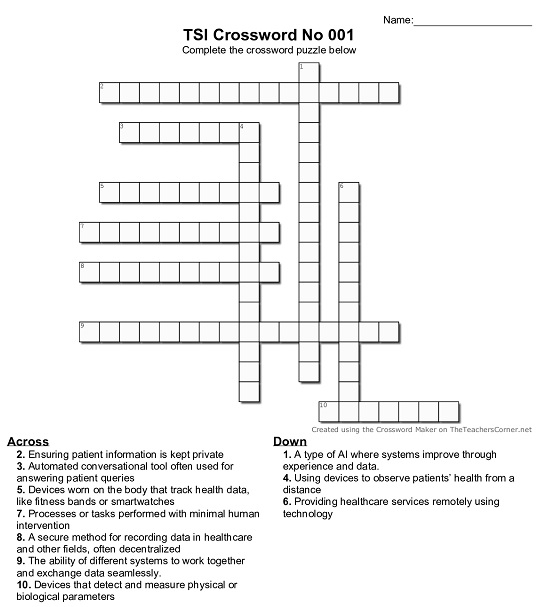
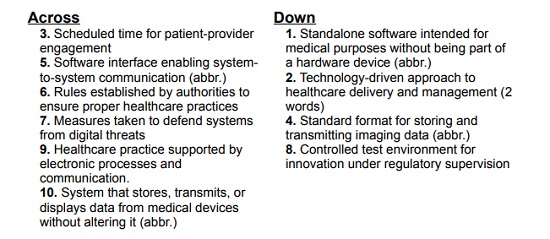
The month of June has been relatively quiet for TSI, but we’ve curated a few interesting articles in this newsletter to keep you engaged. Dr. Umasankar, our dynamic Secretary, continues to contribute his popular medical-technology crosswords – hope many of you are taking part! The solution to the May crossword is also included in this issue.
Looking ahead, our Annual Meeting in Bangalore is scheduled for the last week of November 2025. We encourage all members to start registering early and help make the event a grand success.
Thank You
Dr. Sunil Shroff
Chief Editor
President-Elect, TSI

Telemedicine in Diabetes Practice: Revolutionizing Chronic Disease Management
Dr. Sunil Shroff
President-Elect, Telemedicine Society of India | Consultant Urologist & Transplant Surgeon
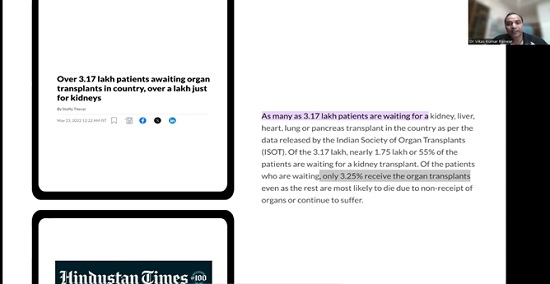
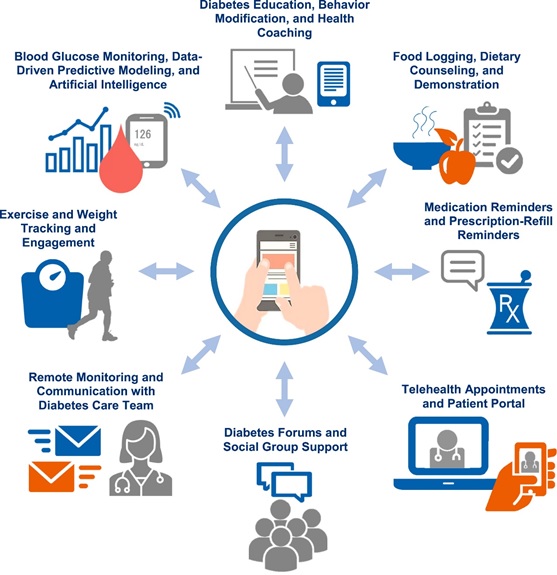
Telemedicine has been a blessing for chronic disease management. Among the many fields it has transformed, diabetes care stands out due to the continuous and proactive management it requires. Diabetes as we are aware is a chronic condition that affects a large population with over 500 million people worldwide. India is known as diabetes capital of the world.
Most dialectologist practitioners have monitored their patient using telephone or sms messages or Whatsapp – hence telemedicine has only added to the ease and this has further been made easy with availability of many diabetes specific apps, it has become ever so easy to manage this condition. Hence the integration of telemedicine in diabetes practice has significantly improved patient outcomes, accessibility, and the efficiency of healthcare delivery.
Effective management of diabetes hinges on regular monitoring of blood glucose levels, lifestyle modifications through constant reminders and nudges, medication adherence, and frequent communication between patients and healthcare providers. Traditionally, this has involved frequent in-person visits. However, telemedicine has introduced a paradigm shift by enabling remote monitoring, virtual consultations, and real-time data sharing between patients and clinicians.
One of the core advantages of telemedicine in diabetes care is improved access, especially for patients in rural or underserved regions. Geographic barriers and limited mobility often prevent consistent follow-up visits. With telemedicine, patients can connect with clinicians like endocrinologists, diabetes educators or coaches, and dietitians from the comfort of their homes. This reduces the burden of travel, saves time, and ensures that more people receive regular care.
Technology plays a central role in this model. Continuous glucose monitors (CGMs), smart insulin pens, and mobile apps allow patients to track their blood glucose levels and insulin usage in real-time. These data can be automatically uploaded to cloud-based platforms, where healthcare providers can review trends and make timely adjustments to treatment plans. Video consultations enable providers to explain changes, answer questions, and provide personalized counseling, maintaining a high standard of care without the need for face-to-face interaction.
Telemedicine also empowers patients to take an active role in managing their condition. Educational resources and virtual coaching can be delivered through telehealth platforms, increasing patient engagement and understanding of the disease. For individuals newly diagnosed with diabetes, virtual onboarding sessions can provide essential training on glucose monitoring, insulin administration, and dietary guidance.
During the COVID-19 pandemic, the value of telemedicine in diabetes care became especially evident. With limited access to clinics, many healthcare systems adopted telehealth tools out of necessity, leading to an acceleration in digital health adoption. Patients and providers alike discovered the convenience and efficacy of remote diabetes management, prompting a lasting shift in care models even after the pandemic subsided.
Despite its benefits, telemedicine in diabetes practice also presents challenges. Not all clinicians are aware of the regulatory requirement to practice telemedicine in India. And not all patients have access to reliable internet or digital devices, and some may lack the technological literacy needed to effectively use remote care tools. Practitioners can take a short online course to familiarising themselves with telemedicine guidelines as prescribed by National Medical Council that is available at subsidized cost.
In conclusion, telemedicine has become an indispensable component of modern diabetes management. It offers a more accessible, efficient, and patient-centered approach to care, especially for individuals with chronic needs. As digital health technology continues to evolve, and healthcare systems adapt to hybrid models of care, telemedicine is set to play an even more prominent role in shaping the future of diabetes practice.

Diabetes and Telemedicine Practice Online Course
Ms. Preeti Jha
Course Coordinator
Telemedicine Courses – TSI
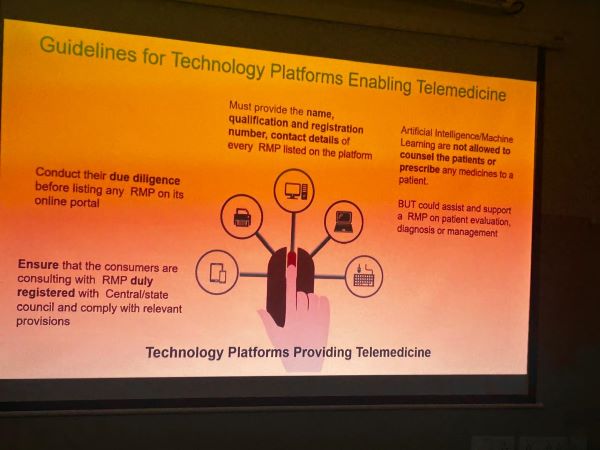
Diabetes Telemedicine Practice Course has been put together by experts in the field who are familiar with this form of practice for many years. This course follows the same level of compliance as available in the document released by the Ministry of Health & Family Welfare, Government of India entitled ‘Telemedicine Practice Guidelines.
The diabetes course helps the diabetes practitioners to understand the requirements for such a practice. Some of the faculty of this course are members of Telemedicine Society of India, however it is not administered by TSI. The course directors are Dr.V. Mohan from Chennai & Dr. Jothydev Kesavadev from Trivandrum.
This course was launched Telehealth Diabetes online course for medical practitioners on the 30th July 2023 during the 8th Edition of Dr.Mohan’s International Diabetes Update.
Once you register your login and password will be issued along with an e-book about the Telemedicine Practice Guidelines. This contains the Ministry guidelines along with a set FAQ’s.
We highly recommend that you go through the Telemedicine Practice Guidelines and the FAQ’s before you watch the course video lectures.
There are also optional course videos available for you and these will help you not only enhance your knowledge but also improve your communication skills for teleconsultations.
Target audience: Medical Doctors who are practicing diabetes and providing teleconsultations
Online Platform: MOODLE
Webinar Delivery: Via Online Platform
Structure and Format
Pre-assessment – 20 mins – Compulsory
Module I. Introductory Primer to Tele-Diabetes
1. Definitions of Terminology in Telemedicine (Compulsory) -15 mins
2. Telehealth and Diabetes Introduction Page
Video Lectures
Lecture 1: Telemedicine for diabetology experiences
Lecture 2: Telemedicine Practice Guidelines by GOI (Compulsory)
Module II – Setting up a Diabetes & Telehealth Practice
PowerPoint presentations
1. Telemedicine for Diabetes Care: Case Based Approach
2. Telemedicine for Diabetes Care: Practical Tips on How to set up a Telehealth Facility
3. Telemedicine and Foot care in Diabetes
Video Lectures
Lecture 3: Telemedicine- Communication & Tips-(Highly recommended) – 20mins
Lecture 4: Implementing Technology in Diabetes via Telemedicine
Frequently Asked Questions in setting up telemedicine consultations-
(A Primer in the form of Q & A (Highly recommended)-60mins)
General Questions on Telemedicine
Skills related questions and resources
Consultation related question
Gadgets
Module III. Legal & Ethical Aspects
1. Telemedicine Practice Guidelines by Ministry of Health – PPT (Compulsory) – 30mins
Video Lectures
Lecture 5: Ethical code of conduct INDIAN MEDICAL COUNCIL (Highly Recommended) – 30mins
FAQ’s of BoG from MCI
FAQs on Telemedicine Practice Guidelines from MCI – From RMP/ Care-givers’ point of view
FAQs on Telemedicine Practice Guidelines from MCI – From Patients/Care-seekers’ point of view
Module IV. Optional Reading Material
Indian Medical Council Regulations(Recommended reading)
Diabetes-related research papers
Problems associated with diabetes care in India
Diabetes Mellitus and Peripheral Vascular Disease
Diabetic foot related research papers
Knowledge, attitude, and practice of foot care in patients with diabetes at central rural India
Diabetic Foot Infection: An Indian Scenario
The global burden of diabetic foot disease
Management of Diabetic Foot in an Indian Clinical Setup: An Opinion Survey
Feedback – Compulsory
Duration: The course would take a total of 4 to 6 hours to complete and you can do it at your own pace.
The login and password will be available to you for a period of one year from date of registration and payment and there are no limits to your viewing the course.
Assessment: There are pre-course and post course assessments. Each question can be attempted only once.
Post course Assessment – compulsory (40 mins)
Certification of Participation or Certificate of Proficiency: After completion of the course, including faculty interaction you may take the assessment, after which depending on the performance you will get either the Certification of Participation or Certificate of Proficiency.
A short video of the course is included below. Those interested in taking up this course please click on the link – https://doctorguru.com/register-diabetes-course.asp

AI Tool Identifies Heart Risk Using Archived Scans
Colleen Fleiss
M.SC (Bioinformatics)
Content Writer, Medindia.net
AI analyzes medical data (scans, EHRs) to detect heart disease early, predict risks, and personalize treatments.
Researchers at Mass General Brigham, in partnership with the U.S. Department of Veterans Affairs, have created an AI tool that analyzes existing CT scans to detect elevated coronary artery calcium (CAC) levels – a key indicator of increased risk for heart-related events.
Published in NEJM AI, the study showed the tool, named AI-CAC, accurately predicted future heart attacks and 10-year mortality. The results highlight its potential to support clinicians in evaluating long-term cardiovascular risk across broader populations.
Unlocking Hidden Cardiac Risk
“Millions of chest CT scans are taken each year, often in healthy people, for example to screen for lung cancer. Our study shows that important information about cardiovascular risk is going unnoticed in these scans,” said senior author Hugo Aerts, PhD, director of the Artificial Intelligence in Medicine (AIM) Program at Mass General Brigham.
“Our study shows that AI has the potential to change how clinicians practice medicine and enable physicians to engage with patients earlier, before their heart disease advances to a cardiac event.”
Chest CT scans can detect calcium deposits in the heart and arteries that increase the risk of a heart attack. The gold standard for quantifying CAC uses “gated” CT scans, that synchronize to the heartbeat to reduce motion during the scan. But most chest CT scans obtained for routine clinical purposes are “nongated.”
The researchers recognized that CAC could still be detected on these nongated scans, which led them to develop AI-CAC, a deep learning algorithm to probe through the nongated scans and quantify CAC to help predict the risk of cardiovascular events. They trained the model on chest CT scans collected as part of the usual care of veterans across 98 VA medical centers and then tested AI-CAC’s performance on 8,052 CT scans to simulate CAC screening in routine imaging tests.
AI Accurately Predicts Cardiovascular Risk
The researchers found the AI-CAC model was 89.4% accurate at determining whether a scan contained CAC or not. For those with CAC present, the model was 87.3% accurate at determining whether the score was higher or lower than 100, indicating a moderate cardiovascular risk.
AI-CAC was also predictive of 10-year all-cause mortality—those with a CAC score of over 400 had a 3.49 times higher risk of death over a 10-year period than patients with a score of zero. Of the patients the model identified as having very high CAC scores (greater than 400), four cardiologists verified that almost all of them (99.2%) would benefit from lipid lowering therapy.
“At present, VA imaging systems contain millions of nongated chest CT scans that may have been taken for another purpose, around 50,000 gated studies. This presents an opportunity for AI-CAC to leverage routinely collected nongated scans for purposes of cardiovascular risk evaluation and to enhance care,” said first author Raffi Hagopian, MD, a cardiologist and researcher in the Applied Innovations and Medical Informatics group at the VA Long Beach Healthcare System.
“Using AI for tasks like CAC detection can help shift medicine from a reactive approach to the proactive prevention of disease, reducing long-term morbidity, mortality and healthcare costs.”
Limitations to the study include the fact that the algorithm was developed on an exclusively veteran population. The team hopes to conduct future studies in the general population and test whether the tool can assess the impact of lipid-lowering medications on CAC scores.

AI-Driven Flexible Wristband Tracks Breathing Patterns With High Accuracy
Naina Bhargava, MPharm (Master of Pharmacy)
Content Writer, Medindia.net
A flexible wristband with a fingertip-inspired sensor and AI decoding can track breathing patterns with over 99.5% accuracy.
A lightweight, flexible wristband can now accurately decode breathing patterns by analyzing pulse signals, achieving over 99.5% accuracy with the help of a fingertip-inspired pressure sensor and deep learning. Developed by a team including researchers from North University of China and Xiamen University, this system offers an effortless and unobtrusive alternative to bulky chest straps or nasal devices, enabling continuous, real-time respiratory monitoring. This breakthrough could transform respiratory care, especially for individuals managing chronic conditions or recovering from illness.
Chronic Respiratory Diseases and Monitoring Challenges
Chronic respiratory diseases affect millions globally and require constant monitoring to manage symptoms and prevent complications. However, existing technologies – such as chest belts or nasal prongs – can be intrusive and unsuitable for long-term daily use. Recent approaches have explored indirect signals like heart rate or pulse waveforms, offering better comfort but often sacrificing accuracy.
Traditional signal classification methods fall short when faced with the complexity of human respiration. Due to these challenges, there is a growing demand for devices that are not only comfortable to wear but also capable of extracting high-fidelity respiratory data over extended periods. Based on these challenges, there is a pressing need to develop advanced systems for long-term, precise respiratory monitoring.
Innovative Wearable System With Artificial Intelligence
Researchers from North University of China and Xiamen University have unveiled a novel wearable system that reads respiratory patterns directly from wrist pulse signals. Published in Microsystems & Nanoengineering, the study details a miniaturized, AI-powered device that integrates a flexible pressure sensor with a deep neural network. The sensor system enables continuous respiratory tracking with high comfort and clinical-grade precision, offering a promising alternative to traditional respiratory monitors.
Fingertip-Inspired Sensor and Deep Neural Network Design
At the heart of the system lies a 300-μm-thick flexible pressure sensor, inspired by the structure of a human fingertip. Printed on a thermoplastic polyurethane (TPU) substrate, the sensor is capable of detecting subtle fluctuations in pulse waves caused by respiration.
These signals-categorized as respiration-induced amplitude variation (RIAV), respiration-induced fluctuation in ventricular filling (RIFV), and respiration-induced variation in baseline (RIIV)-are transmitted to a mobile application via Bluetooth and processed using a hybrid Residual Network – Bidirectional Long Short-Term Memory (ResNet-BiLSTM) neural network. This deep learning model captures the temporal and spatial dynamics of respiratory patterns, classifying slow, normal, fast, and simulated breathing states with a remarkable 99.5% accuracy.
Lightweight Design and Real-World Testing
The device’s ultra-lightweight construction (just 9 grams), skin-conforming design, and long-term mechanical stability allow it to be worn for hours without discomfort.
Testing involved 13 human volunteers and machine-simulated breathing, demonstrating the sensor’s robustness across real and artificial respiratory scenarios. By avoiding reliance on chest placement or airflow proximity, the device simplifies setup and enhances usability-making it ideal for users in everyday environments.
Potential Impact on Chronic Disease Management
“Our mission was to bridge the gap between high-precision monitoring and wearable comfort,” said Dr. Libo Gao, senior author of the study. “We’ve shown that you can track respiration with clinical accuracy-without putting anything on your chest or face. This could be a game-changer in how we approach remote health monitoring, especially for patients who need round-the-clock care.”
The device’s ability to deliver accurate respiratory insights in a comfortable, wearable format opens new doors for chronic disease management, eldercare, and telemedicine. Its seamless integration with mobile platforms allows for real-time alerts and long-term data logging-tools that are essential for early intervention in conditions like COPD or sleep apnea. Beyond healthcare, this innovation could also benefit athletes, astronauts, or high-altitude workers by offering continuous respiration tracking in dynamic environments. As wearable tech evolves, this wrist-worn system could become a cornerstone in the future of personalized respiratory health monitoring.

When AI Sings and Friends Speak: MediBuddy’s Musical Mission to Stub Out Smoking
Colleen Fleiss
M.SC (Bioinformatics)
Content Writer, Medindia.net
Quitting smoking boosts lung health, improves heart function, and protects loved ones from secondhand smoke.
In a bold and innovative step toward promoting public health, MediBuddy, India’s leading digital healthcare platform, has launched its latest awareness campaign, #NoPuffPlease,. Departing from traditional, fear-based public service messages, this campaign hinges on a compelling AI-generated anti-smoking anthem titled “Love You Bro… But Not Your Smoking.”
Unlike the grim tone often associated with anti-smoking campaigns, MediBuddy takes a creative leap by engaging technology and music to create impact. The anthem – completely written, composed, and produced using artificial intelligence tools – captures the emotional nuance of a friend urging another to quit smoking, not through judgment, but through concern.
Blending Hinglish lyrics with a street-style beat, the song is catchy, conversational, and easy to share – designed specifically to connect with younger audiences aged 15–24, who represent a significant portion of India’s smoking demographic. The anthem avoids preaching and instead delivers its message in the voice of peers – a choice that makes it feel authentic and relatable.
“We wanted to go beyond scare tactics and speak directly to young adults in a way that’s fun, emotional, and thought-provoking,” said Manu Sankar Das, Head of Brand Marketing at MediBuddy. “Using AI to build this anthem from scratch allowed us to create something culturally relevant and impactful.”
A Wake-Up Call on Secondhand Smoke
The campaign sheds light on the deadly effects of passive smoking. According to 2024 WHO data, more than 40% of non-smokers are regularly exposed to secondhand smoke, especially in homes and public places. This exposure leads to nearly 1.2 million deaths globally every year, with India among the top contributors.
The Global Adult Tobacco Survey (GATS) highlights that over 267 million Indians use tobacco, with 28% of adults aged 15–24 smoking regularly. These numbers underscore the urgent need for campaigns like #NoPuffPlease that not only promote quitting but also encourage social accountability.
By framing smoking as something that harms relationships – not just lungs – MediBuddy transforms a difficult topic into an emotional, relatable conversation. With “Love You Bro… But Not Your Smoking,” the company is encouraging friends and families to speak up, creating a ripple effect of collective action.
The campaign is live across social platforms, inviting users to share the song, tag friends, and spread the message using #NoPuffPlease. As India marks World No Tobacco Day, MediBuddy redefines public health messaging with rhythm, empathy, and AI-driven creativity – making it easier, and cooler, to say: quit smoking for yourself and for everyone around you.
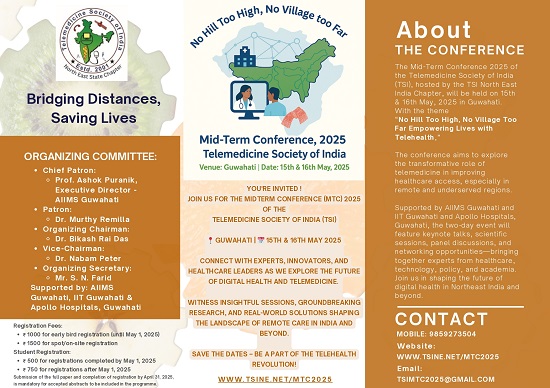
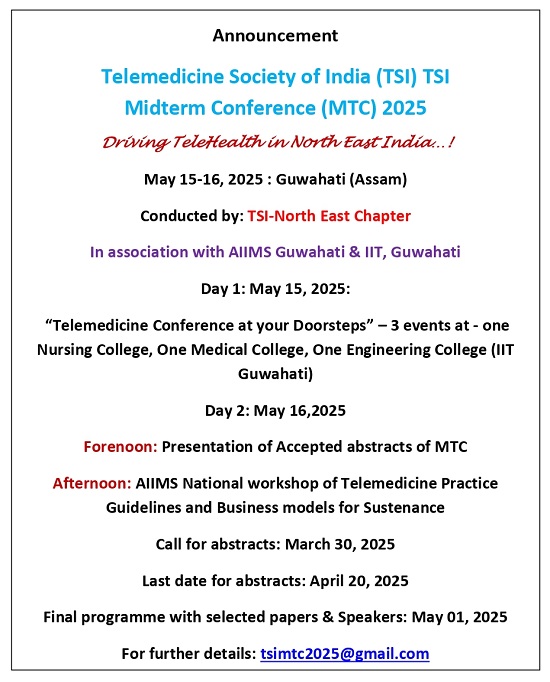
::ANNOUNCEMENTS::
::CROSSWORD::
Telemedicine – News from India & Abroad
Could AI Understand Your Tumour Better Than a Doctor?
AI offers hope for smarter, more targeted therapies in breast cancer by uncovering the hidden diversity of cancer cells………. Read More
Can AI-Powered Meal Plans Help Cancer Patients Eat Better?
AI tools like ChatGPT and Gemini may soon help bridge nutrition gaps in cancer care by offering culturally sensitive………….. Read More
AI Sets New Standard in Radiology Accuracy and Efficiency
The Northwestern team is refining AI to catch missed or delayed diagnoses like early-stage lung cancer………… Read More
Face the Future: AI Reads Facial Palsy Like a Plastic Surgeon
AI-powered 3D-FAN model enhances facial recognition with high accuracy and 3D feature mapping…… Read More
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
Medical Writing Certificate Course with Internship Opportunity!
TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TSI Newsletter-
- Report can be from 500 to 600 words
- Report Should be relevant to Telemedicine or Medical Informatics
- No promotion of self or any product
- Avoid plagiarism
- All references should be included
- Provide any attributions
- Visuals are welcome including video links
- Send full authors name, degrees, affiliations along with a passport sized photograph of good resolution. If multiple authors only main author photo to be sent.
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net