Telehealth Newsletter
Official Newsletter of Telemedicine Society of India

What is New?
The month of March saw a dip in telehealth activities, though we have covered the Apollo Telehealth event in detail. In this newsletter, we focus on an interesting area of smart hospitals that are already revolutionizing patient care-and soon, they will make significant inroads into India.
In addition, we share the inspiring story of Eric Lefkofsky, the billionaire entrepreneur behind Groupon, who turned personal adversity into groundbreaking innovation. In 2014, after his wife Liz was diagnosed with breast cancer, Eric was struck by the limited use of data in critical oncology decision making. Determined to change this, he founded Tempus, an AI-powered precision medicine company that now processes over 50,000 patient samples monthly and has grown to an $8.1 billion valuation. His journey from crisis to innovation exemplifies how technology can be harnessed to revolutionize healthcare. For more insights, be sure to watch his recent interview on YouTube – the link is provided in our newsletter.
As we head into the summer months, with temperatures expected to peak, we encourage everyone to take extra care and stay cool.
Stay tuned as we continue to explore the latest trends and success stories shaping the future of healthcare. Do contribute, and get your events documented. We wish Odhisha Chapter the very best for the upcoming telemedicine state chapter conference.
Thank You
Dr. Sunil Shroff
Chief Editor
President-Elect, TSI
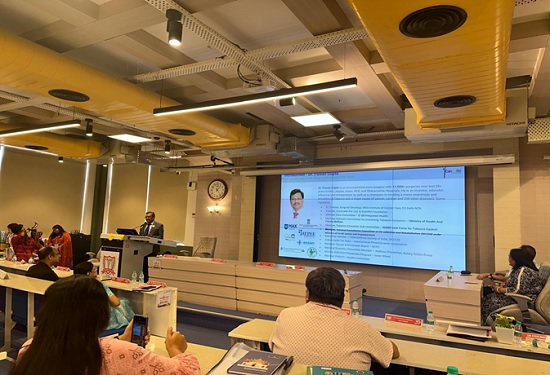
Revolutionizing Healthcare: The 12th International Conference on Transforming Healthcare with IT
Apollo Telemedicine Networking Foundation
In a landmark event redefining the intersection of healthcare and digital innovation, the 12th International Conference on Transforming Healthcare with IT unfurled its dynamic agenda on the 21st and 22nd of February, 2025, at the esteemed Bharat Mandapam, New Delhi. Under the compelling theme “From Hype to Hope: Establishing a Digital Health Landscape,” this transformative conclave, spearheaded by the Apollo Telemedicine Networking Foundation and Apollo Hospitals, convened an elite cadre of global pioneers in healthcare and information technology. The gathering served as an incubator for groundbreaking discussions, unveiling cutting-edge advancements poised to redefine the contours of modern medicine. The event witnessed the participation of over 7,000 delegates, 400+ speakers, and 200+ innovators, making it one of the most impactful healthcare IT conferences to date.
A Visionary Convergence for Digital Healthcare Evolution
The core ambition of this high-calibre symposium was to delineate the manifold ways in which information technology can propel healthcare into an era of heightened efficiency, precision, and accessibility. By fostering dialogue among experts, the event spotlighted emerging trends, persistent challenges, and pioneering solutions within healthcare IT. The deliberations centred on harnessing digital breakthroughs to refine patient care, optimize clinical workflows, and curtail operational expenditures.
Key Features of the Conference
Illuminating Keynote Sessions
A constellation of influential thought leaders, including Shri Jagat Prakash Nadda, Dr Subrahmanyam Jaishankar, Dr Jitendra Singh, Dr Sangitha Reddy, and Health Ministers representing Maldives, Guyana, Fiji, and Eswatini, delivered riveting keynote addresses. These luminaries expounded upon critical themes such as artificial intelligence in healthcare, cybersecurity imperatives, and the expansive reach of telemedicine. Their discourse underscored the transformative prowess of technology in sculpting the future of global healthcare systems.
Dynamic Panel Discussions
Interactive panel dialogues facilitated robust engagement among attendees and industry stalwarts, delving into pivotal topics such as digital health records, big data analytics, and interoperability solutions. These sessions served as crucibles for idea exchange, fostering cross-disciplinary collaborations that promise to drive the next wave of healthcare advancements.
Strategic Networking Opportunities
The conference provided a fertile ground for forging meaningful professional alliances, offering participants an invaluable chance to connect with peers, visionaries, and potential collaborators. These interactions catalyzed the genesis of strategic partnerships and set the stage for long-term synergies in healthcare innovation.



Pivotal Outcomes and Industry Advancements
Enriching Knowledge Exchange
Attendees gained unparalleled insights into the latest healthcare IT paradigms, equipping them with actionable intelligence on leveraging technological prowess to refine medical delivery and patient management.
Catalyzing Collaborative Initiatives
The event functioned as an accelerator for cooperative endeavours, facilitating groundbreaking partnerships between healthcare institutions, technology firms, and policy architects. These alliances are expected to seed transformative projects aimed at reshaping healthcare landscapes globally.
Showcasing Revolutionary Solutions
Innovative technological marvels took centre stage, with AI-driven diagnostic systems, blockchain-powered patient data security solutions, and state-of-the-art telehealth platforms emerging as the highlights of the conference. These cutting-edge tools exemplify the potential of digital integration in enhancing healthcare accessibility and efficiency.
Trailblazing Approaches Elevating the Conference Experience
Immersive Virtual Reality Demonstrations
Pioneering the integration of experiential technology, the event featured Virtual Reality (VR) showcases, allowing attendees to engage with avant-garde healthcare IT solutions in a deeply immersive manner. This hands-on exploration brought theoretical innovations to life, offering tangible perspectives on their real-world applicability.
The “Solvathon” Hackathon
A riveting 36-hour hackathon, aptly dubbed “Solvathon,” convened a coalition of students, developers, and healthcare IT trailblazers. Participants were tasked with devising ingenious solutions to real-world healthcare dilemmas. The most promising innovations were spotlighted on the conference stage, celebrating technical ingenuity and problem-solving acumen.
Hybrid Format for Expanded Reach
Embracing inclusivity, the conference adopted a hybrid model, blending physical attendance with virtual participation. This format ensured broader accessibility, allowing professionals from across the globe to partake in the intellectual discourse and knowledge dissemination.
Live-Streaming for Unparalleled Accessibility
To democratize access to these invaluable discussions, conference sessions were broadcast live, enabling remote audiences to engage with thought leaders and industry experts in realtime.
Looking Ahead: The Future of Healthcare IT
In summation, the 12th International Conference on Transforming Healthcare with IT emerged as an unequivocal triumph, serving as a crucible for innovation, collaboration, and intellectual exchange. The event reaffirmed the indispensable role of digital technology in sculpting a more efficient, patient-centric healthcare ecosystem. With great anticipation, we look forward to the 13th edition of this trailblazing conference, where the journey of digital transformation in healthcare will continue to break new frontiers.
Video Link: Transforming Health with IT 2025 | Revolutionizing Healthcare Through Technology

Smart Hospitals: Revolutionizing Healthcare for a Digital Future
Dr. Sunil Shroff
President-Elect, Telemedicine Society of India | Consultant Urologist & Transplant Surgeon
Smart hospitals represent the future of healthcare by harnessing advanced technologies to deliver more effective and efficient patient care. These innovative institutions integrate artificial intelligence, IoT devices, robotics, and data analytics to revolutionize daily operations and treatment processes. By utilizing real-time data from sensors, wearable devices, and electronic health records, smart hospitals enable proactive monitoring and personalized care plans, ensuring timely interventions in critical situations.
Automation of routine tasks, including scheduling, billing, and maintenance, streamlines operations and allows medical staff to focus on patient outcomes. Artificial intelligence also enhances diagnostic accuracy by analyzing large volumes of medical data and identifying patterns that indicate early signs of illness.
Furthermore, remote monitoring and telemedicine capabilities extend healthcare services beyond traditional hospital settings, providing care for patients in rural or underserved areas. Data-driven decision-making optimizes resource allocation and treatment protocols, reducing hospital stays and operational costs. With a focus on improving patient safety and experience, smart hospitals are poised to transform the healthcare landscape, making it more responsive, efficient, and patient-centered. Embracing these technologies now promises a future where medical care is continuously evolving to meet the demands of an increasingly digital world. This transformation ultimately leads to significantly better outcomes for all.
Watch the YouTube Video from China about Smart Hospitals
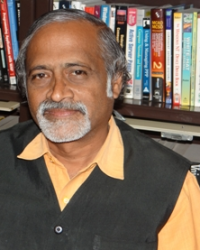
The video showcases various automated systems operating within a modern hospital, presented as part of “China’s Smart Hospital Revolution.”
- Overhead Rail Delivery System: Small, boxy robotic units travel along tracks installed on the ceiling. They navigate corridors, make turns, and appear to transport items (presumably medicines or small supplies) between locations, such as from a central pharmacy to a nurse station (a sign for “Nurse Station” is visible). Some units have digital displays.
- Automated Pharmacy Storage/Retrieval: Inside what looks like a pharmacy storage area with floor-to-ceiling shelves packed with medicine boxes, a large robotic system with an arm moves vertically and horizontally to select and retrieve specific packages.
- Pharmacy Dispensing: At a pharmacy counter, retrieved medicines arrive via a large spiral chute system, delivering them down to a waiting pharmacist or technician who collects them in a basket.
- Floor-Based Autonomous Mobile Robots (AMRs): Different types of robots are shown moving autonomously along hospital corridors on the floor. One robot carries a multi-tiered cart loaded with linens or supplies. Staff can be seen working alongside these robots, with one person even riding a small electric bike/scooter in the same hallway.
- Automated Injection Preparation: A close-up shows a robotic arm precisely handling vials and a syringe, seemingly preparing an injection automatically.
Overall, the video highlights the integration of advanced robotics and automation for tasks like medicine retrieval, transport, dispensing, supply logistics, and potentially even medication preparation within a Chinese hospital setting, aiming to improve efficiency.

Efforts to Expand Telemedicine Services and TSI in North Eastern Region of India
Dr. Murthy Remilla
Vice-President, Telemedicine Society of India
As TSI members are aware, we have a North-East Chapter of TSI from Oct 2023, headquartered at Guwahati. Generally, a minimum of 20 members are required to start a state chapter. However, in the case of north east comprising the states of Arunachal Pradesh, Assam, Manipur, Meghalaya, Mizoram, Nagaland and Tripura (commonly known as the “Seven Sisters”), and the “brother” state of Sikkim was considered special by the TSI EC and approved forming a chapter for the 8 chapters together to kickstart the activities. The plan is to slowly expand to as many individual state chapters as possible with 20 members from each state particularly, two big states among them viz., Assam and Arunachal Pradesh. Though the chapter was formed more than a year and half, significant activity is yet to take off.
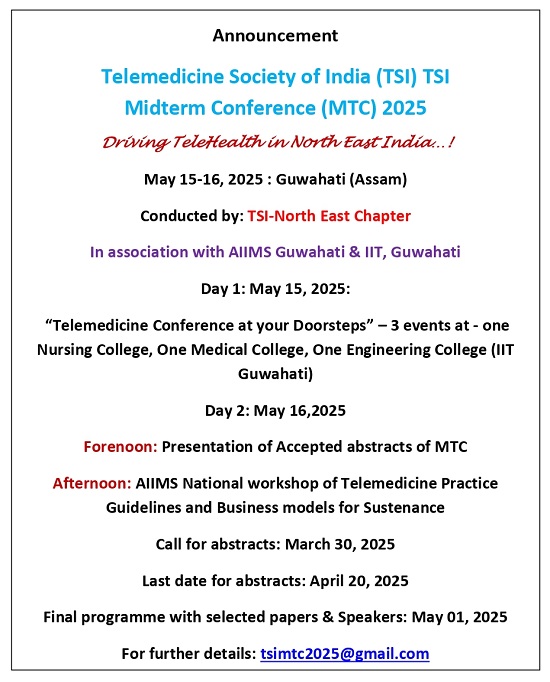
I had been to Itanagar (Arunachal Pradesh) and Guwahati (Assam) personally recently to have personal discussions and motivate and mobilize the teams and also to encourage them to hold this year’s Mid-Term Conference at in the region. The preliminary discussions brought out the fact that, Guwahati is the big city of the region and with good access by road, air and rail. Guwahati also has good number of Medical and Engineering institutions including prestigious AIIMS and IIT.
Had a great Introductory meeting with Dr. Ashok Puranik (Col.) Executive Director AIIMS on March 18,2025. He is very enthusiastic and eager to join TSI and work for the expansion of TM services particularly in NE. When mooted the idea of holding the Midterm meeting of TSI and requested AIIMS to join hands, he has instantly agreed in-principle. To discuss the details and modalities, he was kind enough to give time for a formal meeting along with his TM team the next day where in TSI member Mr. S.N.Farid from Guwahati and AIIMS team of doctors and Telemedicine team participated.
AIIMS also has been thinking of conducting a national workshop on Telemedicine Practice Guidelines (TMPG) for limited numbers as a sort of Training of the Trainers (To). However, on our request it was agreed upon and decided to hold the workshop as part of the Midterm conference to a larger audience during the month of May,2025. AIIMS will be providing the venue and extend best possible support. It was decided to invite as many state government doctors and practioners from all the states of the region and impart this training basically covering- Evolution and Growth of TM in India, TMPG and Ethical and Legal aspects of TM in addition to a talk on the Revenue based business model for TM. ED AIIMS requested a lecture of mine to their medical community and I was fortunate enough to address about 50-60 of them and presented the introduction, status and need for expanding TM Services in the region.

Subsequently, had two wonderful meetings and promising developments at IIT Guwahati where we met two professors Dr. Pradip K Das and Prof. Ajay Dashora who have accepted in principle to be part of midterm conference with one lecture to their Students and faculty on the first day and encouraging their students and faculty for abstracts submission.

Another surprising and unexpected visit was to Mahatma Gandhi University (MGU) at Byrnihat, Ri-Bhoi District Meghalaya. This happened with the personal request and initiative of Dr. Krishna Reedy, Dean of the Unversity. Located about 2 hours drive from Guwahati, nestled amidst the serene hills of Meghalaya, with its recognition from the University Grants Commission (UGC) and approvals from several. professional bodies. Had an occasion to address and interact with MGU’s students of diverse range of courses in the Faculty of Pharmaceutical Science, Nursing department provides ANM and GNM courses, preparing compassionate healthcare professionals, Legal Studies, Allied Health Sciences etc. addressing the growing demand for skilled healthcare professionals. The students also were from the Science & Technology department and Commerce & Management along with Humanities & Social Sciences. Gave the introduction to Telemedicine and how that is more needed and how it can be more useful for their region. The Space Technology based talk was mainly focused and tailored to prepare them for the Telemedicine and rural healthcare services in the backdrop of the infrastructure and affordability for advanced healthcare to that population. Answering the questions from students, information about the proposed midterm conference was given to attract abstracts and participation, but more importantly advised then to take up internships and project works in Telemedicine for different specialties of their studies- Market Potential & Business models; Geographic mapping of Communication and internet availability and zonation of them based on the level of connectivity options; database and mapping of the hospitals and their capacities & specialties; the legal aspects of Telemedicine Practice and any other work for the application of science and Technology for the society. The students were happy (seemed to be happy) with the prospects of potential internships and project works and promised to become students members since I have linked that as a precondition for extending help in internships and project works. Let’s hope for the best and provide our best support whenever they approach, in our own offices or using our contacts in industry. This should be a win-win-win situation for the students, University and TSI as well.


Digitalized Health Insurance: How Technology is Transforming Customer Experiences
Dr. Pavithra S
Assistant Editor, Medindia.net
The health insurance industry is in the middle of a massive digital transformation, triggered by the increasing need for enhanced customer experience. 74% of customers claim they experience problems when trying to buy insurance via the Internet, while 88% say that they want products to be developed for them specifically. Still, 21% of customers think that insurer’s services are not fully personalizable. These figures provide more compelling evidence that cannot go unnoticed by the insurers, and the need to embark on the digital transformation agenda.
AI in Health Insurance
AI is also one of the most vital digital technologies that is being implemented by the health insurance industry. Machine learning analytics delivers relevant customer premiums and risk management plans with up-to-date information for insurance companies. According to the research, the implementation of AI and machine learning is projected to raise labor productivity in the sector to 35% by 2025. In addition, AI in platforms is of great value when it comes to customer relations by providing quick and efficient responses from webchats, and electronic assistants, among others.
Blockchain for Health Insurance
Technological advancement, specifically through blockchain, offers transparency and security to the insurance process. According to a survey conducted in 2019, 66% of the insurers are embracing blockchain to enhance the claim processing and fraudulent control. Blockchain effectively guarantees secure transfer of health data between various stakeholders because the records cannot be tampered with. Also, blockchain supports efficient interaction between various healthcare stakeholders, secondary making communication of data streamlined.
Technologies Leading Change in Health Insurance
Internet of Things (IoT): Smart objects allow for patients’ health status to be collected, with real-time data as vital signs, adherence to taken medications, and conditions of chronic diseases. Consequently, it will be possible for insurers to refine the rates and also to offer targeted care. Analysing current trends, experts predict that the count of smart health devices will exceed 50 billion within the year 2028, which should constitute a fantastic opportunity for insurers.
Cloud Computing: Cloud computing is an indispensable commodity in the insurance business due to its scalability and flexibility. Cloud platforms enable the possibility of accessing the needed data in real-time, and fasten the speed of claim handling. Currently, the COVID-19 crisis is driving more insurance firms to invest in cloud-based solutions, and studies suggest that an average of 55% of insurance companies will focus on cloud technology within 3 years to enable insurance digitalization initiatives.
Advantages of Digitalized Health Insurance
- Improved Efficiency and Reduced Costs: With AI, the insurance companies can scale down their costs of operations in claims and underwriting procedures, while at the same time increasing their speed. It is apparent that the use of technology can shave between 30-40% off of the overall time it takes to process claims.
- Enhanced Customer Experience: Using AI and predictive analytics in developing insurance products creates a customer experience. According to the survey conducted in April 2021, as many as 70% of customers indicated their desire to buy insurance that meets their specific need.
- Better Data Management and Security: Blockchain to guarantee secure transactions and free up cloud computing to store and safeguard personal health information from privacy and regulatory invasions. Due to cyber threats, the world economy lost $6 trillion annually, therefore emphasizing the role of effective cybersecurity.
Challenges and Barriers for Health Insurance Tech
- Resistance to Change and Legacy Systems: Most insurance companies today are hardly modern in terms of IT infrastructure and equipment, which hinders the adoption of new technologies; 60% of responding insurers noted that their company’s biggest problem in embracing digital change was that the current IT infrastructure was outdated.
- Cybersecurity and Regulatory Concerns: Insurers are particularly vulnerable to cyberattacks because they process a huge amount of personal data. According to the survey, cybersecurity requires special attention, and insurers are increasingly concerned about it. 58% of insurers cited the importance of data privacy and regulation as critical.
Digital health transformation goes beyond the mere adoption of technology to reconstruct the health insurance industry. By embracing AI, blockchain, IoT, and cloud computing, insurers can boost efficiency and deliver on customer expectations in today’s society.
Research shows that companies that embark on digital initiatives are 2.5 times more likely to deliver higher value than competitors in terms of customer satisfaction and business returns. This shift is important for the long-term sustainability of any organization and especially for the future in the increasing technological environment.
From Crisis to Revolution: How Eric Lefkofsky Turned Personal Tragedy into a Data-Driven Healthcare Breakthrough
Eric Lefkofsky, a billionaire entrepreneur known for Groupon, founded Tempus after his wife, Liz, was diagnosed with breast cancer in 2014. He was alarmed by the lack of data-driven decision-making in oncology and set out to change it.
In 2015, he built a team of experts to develop AI-powered systems that analyze unstructured medical data. Over the years, Tempus refined its genomic analysis algorithms, secured partnerships with major medical centers, and built one of the largest clinical databases, processing over 50,000 patient samples monthly. The company expanded beyond oncology into psychiatry, cardiology, and infectious diseases, proving the scalability of its model.
Today, Tempus has partnered with 50% of U.S. academic medical centers, raised over $1.3 billion from investors like Google, and reached an $8.1 billion valuation with 2,000+ employees. Most importantly, Liz is now cancer-free.
Lefkofsky didn’t just create another unicorn—he introduced Silicon Valley’s data-driven innovation to healthcare.
You can Watch him speaking in a recent interview on Youtube
Transforming Healthcare: Omar Abdullah’s 2025 Budget Expands AIIMS, Nursing Schools, Universal Health Insurance, and Strengthens Telemedicine
In a groundbreaking move to revolutionize healthcare accessibility, Omar Abdullah’s 2025 budget introduces a comprehensive package aimed at strengthening medical infrastructure, enhancing workforce training, and leveraging technology for better patient care.
Key highlights of the budget include:
- Two New AIIMS: Establishing two additional All India Institutes of Medical Sciences (AIIMS) to improve tertiary care access.
- Ten New Nursing Schools: Expanding medical education and strengthening the healthcare workforce.
- Universal Health Insurance: Providing Rs 5 lakh coverage for all citizens, ensuring financial security in medical emergencies.
- Telemedicine Expansion: A major push towards digital health with enhanced telemedicine infrastructure to bridge the urban-rural healthcare divide.
A Game-Changer for Telemedicine
Recognizing the transformative potential of digital health, the budget prioritizes telemedicine to enhance healthcare delivery, particularly in remote and underserved regions. By integrating telemedicine with traditional healthcare, this budget lays the foundation for a more inclusive, accessible, and technology-driven healthcare system, ensuring quality medical care reaches every citizen, regardless of location.
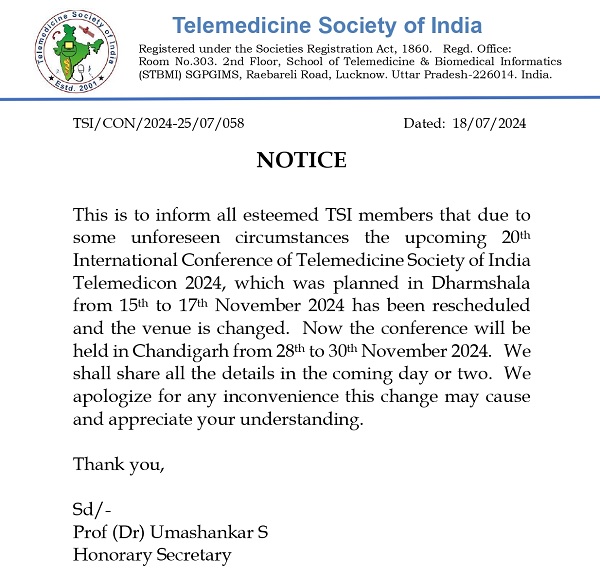
::ANNOUNCEMENTS::


Telemedicine – News from India & Abroad
Unlocking Smarter Heart Health Insights With Smartwatch Data
Wearables track heart function in real time, providing continuous, minute-by-minute health insights Your smartwatch may hold the key to heart health………. Read More
New AI Tool Spots Cognitive Decline
Cognitive impairment in Alzheimer’s affects memory, thinking, and daily functions, worsening over time.Researchers in the US have developed an artificial intelligence………… Read More
Nanotech Meets Smartphone: Rapid Jaundice Detection in Newborns
A portable sensing platform enables quick and accurate jaundice detection for improved health monitoring…….. Read More
India’s AI Revolution: Healthcare Sector Takes the Lead
India’s AI-driven healthcare revolution sets a global benchmark for innovation, efficiency, and inclusivity……….. Read More
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TSI Newsletter-
- Report can be from 500 to 600 words
- Report Should be relevant to Telemedicine or Medical Informatics
- No promotion of self or any product
- Avoid plagiarism
- All references should be included
- Provide any attributions
- Visuals are welcome including video links
- Send full authors name, degrees, affiliations along with a passport sized photograph of good resolution. If multiple authors only main author photo to be sent.
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net