Telehealth Newsletter
Official Newsletter of Telemedicine Society of India

What is New?
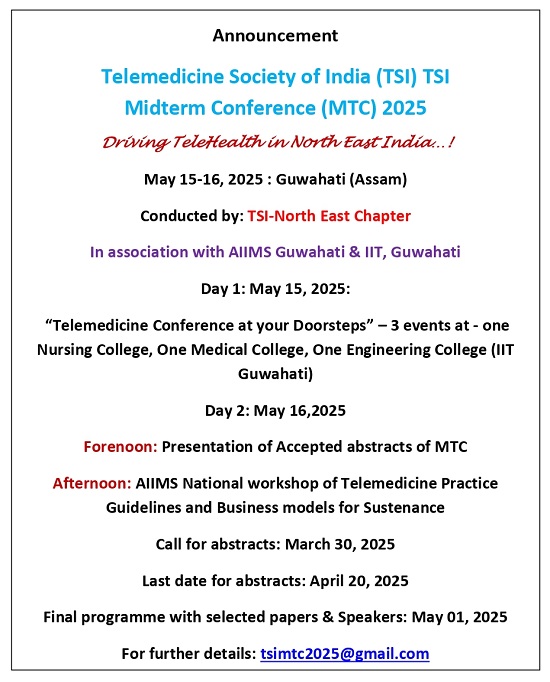
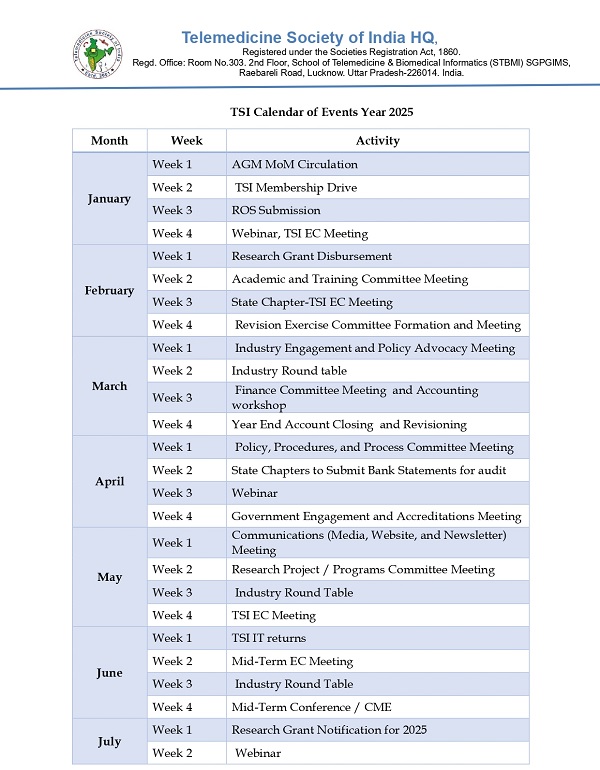
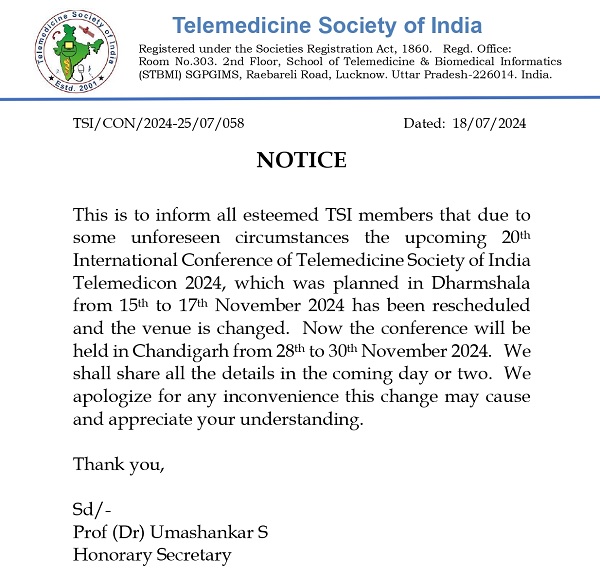
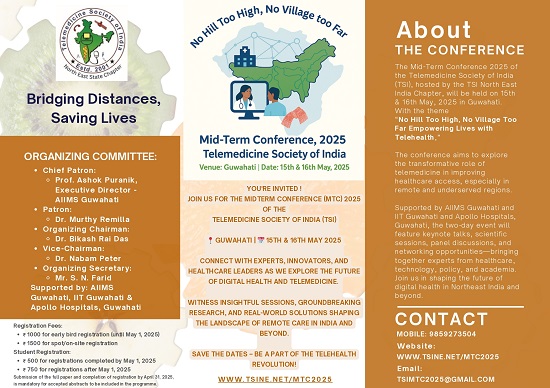
The Telemedicine Society of India (TSI) has two major announcements this year. The mid-term meeting of TSI is scheduled to be held in Guwahati in mid-May, while TELEMEDICON 2025 will take place in India’s IT capital, Bengaluru, at the end of November. Both events promise to be significant milestones in the telemedicine calendar, and more details are included in this newsletter.
We also bring you an engaging report from Dr. B.N. Mohanty, Past President of TSI, who has been a relentless champion for the growth of telemedicine in the state of Odisha. Every April, he organizes the state chapter meeting, and his comprehensive report offers valuable insights into the ongoing initiatives and progress being made.
As we step into the summer months, the soaring temperatures may result in a slight slowdown in field activities. However, this season also presents a great opportunity for the expansion of tele-consultations, allowing healthcare professionals and patients to stay connected while minimizing outdoor exposure.
With the intense heat upon us, we encourage everyone to take necessary precautions – stay well-hydrated, avoid unnecessary outdoor travel during peak hours. Stay cool, stay connected!
Thank You
Dr. Sunil Shroff
Chief Editor
President-Elect, TSI

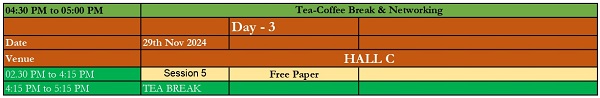
Oditelemedicon 2025 on theme, “Emerging Technologies influencing health care services”
Prof. B.N. Mohanty
Professor Emeritus Endocrine Surgery, Department of Surgery
IMS & Sum Hospital, SOA Deemed to be University Bhubaneswar &
Chief Coordinator Oditelemedicon 2025 | Past President, TSI- Odisha Chapter and Past President-TSI
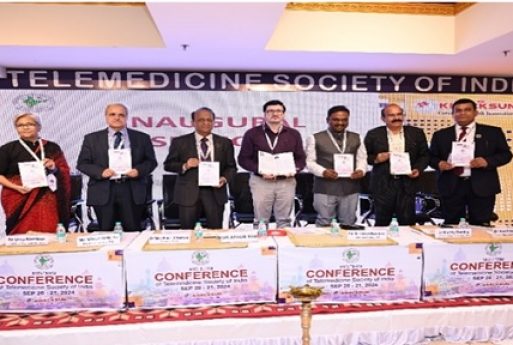
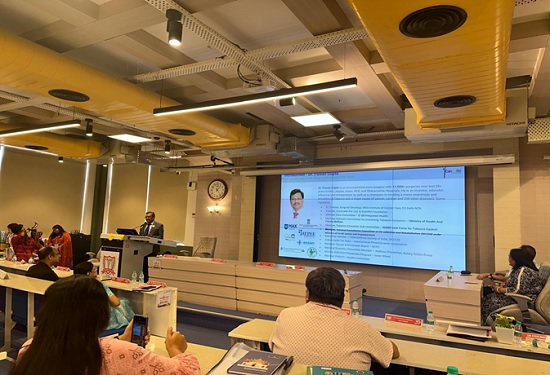
The 13th annual conference of The Telemedicine Society of India (TSI), Odisha Chapter (Oditelemedicon 2025) was organized by TSI, Odisha Chapter in association with District Health Administration, Angul as a hybrid event on 12th April 2025. The venue for the conference was Black Diamond Complex, Angul, Odisha. The theme of the conference was “Emerging Technologies influencing health care services”. A total number of 124 participants from various districts of Odisha physically attended the conference. 17 TSI members attended the conference over virtual platform.
The conference was inaugurated by Mr.Abdaal M Akhtar, IAS, Collector & District Magistrate, Angul. Dr. Umashankar S , Secretary of Telemedicine Society of India attended the inaugural function as guest of honour. Dr. Bijay Kumar Mohapatra, president of TSI, Odisha Chapter presided over the function. Annual Report of the chapter was presented by Odisha Chapter secretary Dr. Sabyasachi Patnaik.
The 1st session was held on ‘Digital Solutions to meet healthcare needs’. The speakers in this session were Dr. B S Ratta, paediatric surgeon from Ruby Hall Clinic, Pune & past-president of TSI; Ms. Madhu Bhatia, Project Manager, DHID from C-DAC, Mohali and Dr.BNR Subudhi, chairman of Ruby Eye Hospital from Berhampur.
The 2nd session was held on ‘Innovations and changing clinical practice’. The speakers in this session were Dr. Pawan Gupta,Sr. Director of Surgical Oncology from MAX Hospital, Delhi NCR; Dr. Bidyut K Das,professor of clinical immunology & rheumatology from SCB Medical College, Cuttack ; Dr. Lucy Patnaik, Associate professor of Radiation Oncology from AH Post Graduate Institute of Cancer, Cuttack and Dr.Anshuman Das, Consultant, Department of Anaesthesia from NALCO Hospital, Angul.
The thematic symposium was held on the theme “Emerging Technologies influencing health care services” at 2.15pm convened by Dr. S K Mishra,Professor of the department of of Endocrine Surgery at Dr. RML Institute of Medical Sciences, Lucknow-cum- past president of TSI. The speakers were Dr. S K Mishra himself; Dr.Alok Modi,Medical Director of Dr Modi’s KEVALYA HOSPITAL from Thane,Maharastra; Dr.Umashankar S, Managing Director of Med.bot , Arogyayati Private Limited from Bangalore and Dr.P K Pradhan,Professor of Nuclear Medicine from SGPGIMS,Lucknow-cum- past president of TSI.
In the closing session held at 3.50pm, Dr.K Ganapathy, distinguished professor of The Tamilnadu Dr MGR Medical University and past-president of TSI delivered a talk on ‘Technological advances in healthcare in 2030: A peep in to the future’.
The chair persons for different sessions were Dr. I B Kar, past-president, TSI Odisha Chapter from Cuttack; Dr. B K Mohapatra, president of TSI Odisha Chapter from Bhubaneswar; Dr. S K Nayak ex-treasurer of TSI Odisha Chapter from Cuttack, Dr. Prabeer Ch. Mohanty, past-president of TSI Odisha Chapter from New Delhi; Dr.Arun K Choudhury, EC Member of TSI Odisha Chapter from Cuttack; Dr. Arun K Mohanty, Vice-President of TSI Odisha Chapter from Cuttack, Dr.Sibananda Mohanty past-president of TSI Odisha Chapter from Angul and Dr.B N Mohanty, past-president of TSI from Cuttack.
Medical Officers and Community Health Officers from various Govt. Hospitals of Angul District; IMA members of Angul & Talcher branch; Teachers of PMP Medical College & Hospital Angul; Medical Officers of NALCO Hospital; Medical Officers of O P Jindal Occupational Health Center of Jindal Nagar Angul; Medical Officers of NSC Hospital Talcher; TSI members and health administrators attended the conference in-person. Members of TSI including past-presidents, current executive committee members and other invited guests participated in the program over virtual platform from different locations.
The Annual General Body Meeting of the TSI, Odisha Chapter was held at the same venue at 1.15pm on 12.04.2025. The following life members of TSI were elected as office bearers of the Odisha state chapter for the term 2025-26.
| President: | Dr. B Nageswar Rao Subudhi, Berhampur |
| Immediate Past-President: | Dr. Bijay Kumar Mohapatra, Bhubaneswar |
| President-elect: | Dr. Arun Kumar Mohanty, Cuttack |
| Vice-President: | Dr. Arun Kumar Choudhury, Cuttack |
| Secretary: | Dr. Biswajit Samal , Angul |
| Jt. Secretary: | Dr. Pranab Sankar Dash, Baripada |
| Treasurer: | Dr. Sarat Kumar Nayak, Cuttack |
| Executive Members (3): | Dr. Bidyut Kumar Das, Cuttack Dr. Sribatsa Kumar Mohapatra, Burla Dr. Sabyasachi Patnaik, Rourkela |
The valedictory function was held at 4.15pm. Newly elected president Dr. BNR Subudhi was installed during the valedictory function. After installation the incoming president spoke about his plan of action for the coming year. The District Health Administration of Angul District represented by CDM & PHO, Angul was felicitated by President of TSI. Chief Coordinator of the conference Dr. B N Mohanty thanked profusely the Collector & District Magistrate of Angul and the district health administration for their overwhelming support to organize the conference. He also thanked all invited speakers. In the valedictory function, president of IMA, Angul branch highly appreciated the TSI, Odisha Chapter for its consistent effort in enhancing the knowledge of medical professionals of different districts of Odisha on the changing spectrum of digital health application and the consequent benefits to the common man.
Glimpses of the Oditelemedicon 2025





DeepTek’s Chest X-ray AI Achieves EU MDR Certification
Dr. Trupti Shirole
BAMS (Bachelor of Ayurvedic Medicine and Surgery)
Content Writer, Medindia.net
DeepTek reports that its Chest X-ray AI solution has been certified as a Class IIb medical device under the European Union Medical Device Regulation (EU MDR).
Chest X-ray AI Solution Helps Identify 20+ Lung Disorders
The purpose of the Chest X-ray AI solution is to help doctors analyze frontal chest X-rays (AP/PA views). With the help of sophisticated machine learning, the solution can identify more than 20 different lung disorders, including rib and clavicular fractures, as well as nodules, lung masses, TB, and pneumothorax.
Furthermore, the solution recognizes a number of medical devices that are frequently seen in intensive care units and inpatient settings, including pacemakers, chest leads, and different tubes, which offer crucial assistance in challenging clinical situations.
This approach can also read pediatric chest X-rays and detect pediatric tuberculosis and pneumonia, hence improving diagnostic capacities in younger populations, which are frequently underserved by traditional AI models.
DeepTek Acquires CE-Mark and Full US FDA CADe Certification
DeepTek can now make its solution available across Europe and other CE-mark-recognized locations, providing a strong tool to boost productivity, decrease diagnostic delays, and promote quality care delivery on a large scale.
Furthermore, it has acquired full US FDA CADe certification, demonstrating its dependability and clinical rigour in medical imaging applications.
The need for such solutions is especially urgent in areas with a high tuberculosis burden and limited access to specialist radiologists. With a rising tuberculosis burden and an increasing radiology workload, CE certification paves the path for implementation in Europe, Asia, Africa, and other CE-marked locations where AI-driven diagnostics are not only helpful but critical.
The technology has been deployed at 325 TB screening sites, supporting national TB programs and public health activities across several geographies.

Heart Fix in a Flash: A Pacemaker You Can Inject and Forget!
Dr. Shanmathi Rajendran
BDS
Content Writer, Medindia.net
Scientists from the United States have developed the smallest pacemaker, which is smaller than a rice grain? This smart device naturally dissolves inside the body after its programming task ends, thus reducing patient risk, recovery time, and surgical procedure complications.
Grain-Sized Pacemaker That Melts Away!
Modern cardiac pacing systems received substantial advancements through the development of small wireless pacemakers. The Nature Communications study published significant findings about fully implantable pacemakers that operated through near-field energy exchange mechanisms tested on tiny animal subjects, unlocking the potential for self-powered cardiac technologies. This breakthrough finding influenced the incorporation of dissolvable components inside the pacemaker, eliminating the barriers faced with traditional devices.
The wireless pacemaker is battery-free, transmitting infrared light via the skin surface. Small, light-sensitive electronic circuits built into the system enable it to receive and process external light signals used for real-time heart rhythm adjustments. The technology removes the requirement for heavy batteries and hazardous wires that commonly appear inside conventional devices. The pacemaker fits seamlessly onto heart surfaces through its thin, flexible construction for precise electrical pulse delivery.
Why It’s Game-Changing?
Traditional pacemakers are effective, but they frequently result in adverse effects, including infections and dislodged lead, which require extra operations to remove them. That’s where the dissolvable pacemaker system comes into play!
The device exists to dissolve naturally within weeks while simultaneously decreasing hospitalization time and lowering medical expenses and surgical procedures. Medical professionals have identified this temporary, non-invasive option as potentially lifesaving for patients who need post-cardiac surgery support particularly among newborns and infants born with congenital defects.
Engineering a Medical Marvel
Biodegradable materials like magnesium, silicon, and polymers form the core structure of the device. Engineers program these components to erode at specific release rates, which determine the patient requirements. The medical device exhibited reliable and safe performance throughout all preclinical tests conducted on small animals. Such an accomplishment within this bioelectronic and transient medical device demonstrates how medicine can benefit from nanotechnology integration!
Future Potential and Clinical Trials
Researchers tested the pacemaker using animal subjects before moving to human trials. This innovation presents the potential to transform the global cardiac care system, which is particularly beneficial for neonatal and pediatric care as permanent devices face challenges related to size and growth requirements. This light-based control system demonstrates the potential of its technology, extending its usefulness in neuromodulation therapy and soft-tissue interventions.
The dissolvable pacemaker delivered through injection has the potential to revolutionize temporary heart rhythm correction by providing safer and less invasive recovery along with quick treatment procedures. This clinical trial breakthrough is drawing global attention and may mark a new milestone in cardiac medicine.
“Heartbeats restored with no trace left behind!”

AI Ushers in a New Era for Tuberculosis Detection
Colleen Fleiss
M.SC (Bioinformatics)
Content Writer, Medindia.net
KIMS Hospitals, Minister Road, has taken a giant leap in the fight against tuberculosis (TB) by conducting its largest-ever artificial intelligence (AI)– driven study on TB detection using chest X-rays (CXRs). The groundbreaking study retrospectively analyzed 16,675 chest X-rays of adult patients using the advanced AI tool qXR, without direct clinician intervention—marking a milestone in AI-powered diagnostics in India.
AI for TB Detection
The primary aim of the study was to evaluate the diagnostic accuracy of AI in detecting pulmonary TB and to measure its alignment with expert radiologists’ interpretations. The findings were striking: the AI tool demonstrated a sensitivity of 88.7%, showcasing its remarkable ability to correctly identify TB-positive cases. Furthermore, the tool exhibited a Negative Predictive Value (NPV) of 97%, confirming its strong reliability in ruling out non-TB cases. With a specificity of 69.1%, the AI met and even surpassed the minimum criteria set by the World Health Organization (WHO) for TB screening tools.
One of the most noteworthy outcomes of the study was the high level of agreement between AI-based assessments and radiologist interpretations. This significant overlap underscores the potential of AI to not only supplement but also strengthen diagnostic accuracy and clinical decision-making—especially in high-burden, resource-limited settings.
Dr. Latha Sarma, Head of Department and Senior Consultant Pulmonologist at KIMS Hospitals, remarked, “The ability of AI to assist in TB detection with such high accuracy is a game-changer, particularly in areas where access to radiology experts is limited. This can have a profound impact on early diagnosis and timely treatment.”
Dr. Chaithanya Isamalla, Senior Consultant Radiologist at KIMS, added, “AI is not a replacement for human judgment, but it is an incredibly powerful tool for first-line screening. It helps streamline workflows and ensures that complex cases get the focused attention they require.”
The study highlights the rapidly evolving role of artificial intelligence in healthcare, particularly in combating infectious diseases like TB. Tools like qXR offer promising opportunities to scale up early detection, reduce diagnostic delays, and ultimately improve treatment outcomes. As the integration of AI into healthcare systems becomes more widespread, KIMS Hospitals’ pioneering work sets the stage for broader adoption of AI technologies in medical diagnostics—ushering in a new era of smarter, faster, and more accessible healthcare.

AI for Early and Accurate Detection of Parkinson’s Disease
Colleen Fleiss
M.SC (Bioinformatics)
Content Writer, Medindia.net
A researcher at the University of Florida has created an innovative open-source AI program, VisionMD, to analyze videos of patients with Parkinson’s disease and other movement disorders. This tool enables doctors to more precisely track subtle motor changes, enhancing patient care and advancing clinical research.
Diego Guarin, Ph.D., an assistant professor of applied physiology and kinesiology in UF’s College of Health and Human Performance, created the software to address the potential risk of inconsistency and subjectivity in traditional clinical assessments.
“Over the years, we have shown through our research that video analysis of patients performing finger-tapping and other movements provides valuable information about how the disease is progressing and responding to medications or deep brain stimulation,” Guarin said. “However, clinicians don’t have the time and personnel to analyze their videos. To address this, we developed software that can deliver useful results with just a few clicks.”
Guarin, a member of the Fixel Institute for Neurological Disease at UF Health, worked closely with neurologists and other clinician-scientists from the Fixel Institute to refine the tool.
VisionMD analyzes standard videos – whether recorded on a smartphone, laptop or over Zoom – and automatically extracts precise motion metrics. The software runs entirely on local computers, ensuring data privacy.
“It’s not cloud-based, so there is no risk of data leaving the network. You can even unplug from the internet, and it still runs,” Guarin said. The tool is already in use globally, with researchers in Germany, Spain and Italy using it to analyze thousands of patient videos as they explore how computer vision can improve movement disorder care.
Florian Lange, a neurologist at University Hospital Würzburg, praised the software’s ability to provide consistent, objective measurements. He and Martin Reich, a neuroimaging professor at University of Würzburg, adapted VisionMD to help them optimize treatment for patients with tremor, particularly those using deep brain stimulation, or DBS, implants.
“A big challenge with many aspects of medicine today is how difficult it is to get objective data, especially with movement disorders like Parkinson’s disease or tremor,” Lange said from his office in Germany. “If the three of us watched the same video of a patient, we might rate the severity at three different levels. But the software gives us precise, unbiased data.”
By recording videos of patients at a variety of stimulator settings, the software identifies which DBS configuration offers the best symptom relief.
“There are millions of possible programming options, but this tool helps us narrow it down quickly and accurately,” Reich said.
As open-source software, the program is freely available to improve and customize.
The team is also working to expand the tool’s capabilities by adding more motor assessment tasks frequently used in clinical settings.
Early adopters say VisionMD’s accessibility and ease of use have the potential to transform movement disorder research and care.
“It takes only a few seconds to process each video,” Guarin said. “We are confident most clinicians will be able to use it, regardless of their technical expertise.”
OpenAI CEO Sam Altman claims Saying ‘PLEASE’ & ‘THANK YOU’ TO CHATGPT costs tens of millions of dollars
A single query in ChatGPT uses enough energy to power a lightbulb for “about 20 minutes.”
This better – if u can
::ANNOUNCEMENTS::


Telemedicine – News from India & Abroad
AI Tool Predicts Heart Risk With Striking Accuracy
Artificial intelligence (AI) is rapidly reshaping the future of healthcare. In a recent breakthrough researchers at Mount Sinai have calibrated ……… Read More
AI Sees Cancer Before Doctors Do
AI tool spots early signs of lung cancer from general practitioner notes, predicting diagnosis 4 months in advance.Lives are saved ,when algorithms listen better than doctors………… Read More
AI Reveals How the Brain Handles Real-Life Conversations
Speaking and listening share neural pathways, with brain activity adapting precisely to words and context during conversation………. Read More
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TSI Newsletter-
- Report can be from 500 to 600 words
- Report Should be relevant to Telemedicine or Medical Informatics
- No promotion of self or any product
- Avoid plagiarism
- All references should be included
- Provide any attributions
- Visuals are welcome including video links
- Send full authors name, degrees, affiliations along with a passport sized photograph of good resolution. If multiple authors only main author photo to be sent.
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net