Click Here to Download PDF Version

Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
|
What is New? We had an excellent webinar on telemedicine technology by Mr. Mathur from Ahmedabad and the report is covered in this newsletter. The self-learning course with live interaction with the course faculty has been already upgraded to Ver.2 with more interactive lecture videos to provide better learning experience. The online self-learning course ‘Train to Practice Telemedicine’ is a foundation course for all practicing RMPs. This month we are also launching a speciality course on diabetes and telehealth with help of Dr. V. Mohan, Dr. Jothydev Kesavadev, and Dr. Sanjay Sharma. Please visit https://tsi.org.in/courses to view all the courses. If you wish to contribute as a TSI member you are most welcome to join us in development and delivery of these courses. Thank You. |
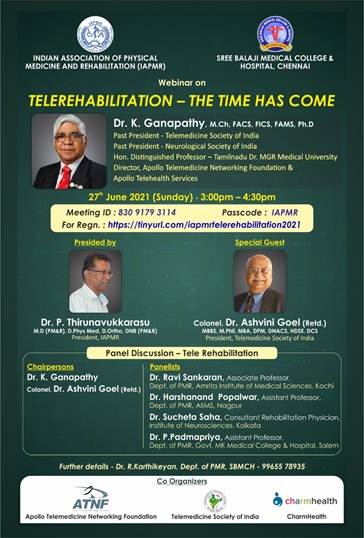
Tele Rehabilitation : The Time has come
 Prof. K. Ganapathy
Prof. K. Ganapathy
Former Secretary and Past President Neurological Society of India, Telemedicine Society of India & Indian Society for Stereotactic & Functional Neurosurgery | Hon Distinguished Professor The TamilNadu Dr. MGR Medical University | Member Roster of experts Digital Health WHO | Director, Apollo Telemedicine Networking Foundation & Apollo Tele Health Services | URL: www.kganapathy.com | EMail: drganapathy@apollohospitals.com
“If I had known I was going to live this long, I would have taken better care of myself.” – Mae West
|
Rehabilitation, the process of restoring an individual to health or normal life through training and therapy, is a major component of Health Sciences. Rehabilitation services have been disrupted due to the COVID-19 pandemic. Even with unlocking and post vaccination, some form of physical distancing is likely to be part of the new normal. This review suggests that, Telerehabilitation (TR) will soon be a distinct stand alone sub speciality of Telehealth and is here to stay. |
Introduction to Telerehabilitation Services
Digitalisation of health care is at an all time high, as is the exponential growth of Telehealth. TR is “the delivery of rehabilitation services via Information and Communication Technologies” . Reduced access to in-person rehabilitation, secondary to the pandemic, is resulting in TR growing exponentially. TR services include evaluation, assessment, monitoring, prevention, intervention, supervision, education, consultation, and coaching. TR services can be deployed across patient populations and multiple healthcare settings including clinics, homes, schools and community-based worksites. A Fortune Business Insights Report estimated a market value of USD 3.32 billion in 2019,with a Compounded Annual Growth Rate (CAGR) of 13.4% leading to USD 9.13 billion by 2027.
Advantages and Barriers in TeleRehabilitation
These include exercising from comfort of home, ability to work on one’s recovery irrespective of time schedule of health care professionals and improved quality of exercise instruction, as they are available for repeated review on video format. Access to high-quality care despite geographical isolation, reduced travel and waiting time, flexibility, and cost-effectiveness are additional benefits Limited computer literacy, unreliable internet connection, language barrier, inability to perform an actual physical assessment, patient privacy, and safety concerns are challenges Some participants were enthusiastic about TR as they could be in contact with their therapist and continue training.
Clinical indications for TR include musculo skeletal disorders, low back ache, spondylosis, osteo arthritis, neck pain ,frozen shoulder and post joint replacement. Neurological conditions benefiting from TR include stroke, neuro trauma, neuro degenerative disorders, cerebral palsy, Post TB Meningitis, neuro muscular disorders, Gullian Barre syndrome, Deuchenne muscular dystrophy and demyelinating diseases. Chronic Obstructive Pulmonary Disorders, post ICU conditions, post Covid, cardiovascular disorders, visual, hearing, developmental disorders, speech and voice dysfunction, swallowing disorders and cognitive dysfunction also benefit from TR . Virtual assessments for pain, swelling, range of motion, muscle strength, balance, gait, and functional assessment demonstrated good concurrence with physical assessments. TR can provide high-quality personalized musculoskeletal physiotherapy. Knee osteoarthritis causes musculoskeletal pain and disability affects up to one-third of people aged over 60 years. Remote muscle strengthening exercises can significantly reduce pain, improve physical function and quality of life. TR for musculo skeletal conditions leads to reduced hospitalization and crowding in physio therapy departments. Musculoskeletal disorders (MSDs) are the second commonest cause of chronic pain and physical disabilities. Physiotherapy assessments that can be done through video include evaluation of pain, swelling, range of motion, muscle strength, balance, gait and functional assessment . TR for stroke, cardiac, pulmonary afflictions and swallowing difficulties
Tele Rehabilitation potential in India
India now has over 100 million senior citizens. The market for geriatric rehabilitation alone is high. Confederation of Indian Industries, in a report showed that 5.5% of seniors were staying at homes. 6% of seniors live alone. Of the 700 million active internet users, 70% access the internet daily mostly using mobiles. Interestingly communication technology is growing faster in rural rather than urban areas. were using smartphones in 2020. 77% of 500 million smartphone users were accessing broadband services. The National Institute of Mental Health and Neuro Sciences (NIMHANS), services delivered telemental health services during the COVID-19 crisis to ensure continuity of care for patients who were unable to avail outpatient services .. A report on 22 senior citizens from four Community Centers in Delhi showed that home-based TR could be used as an adjunct to continue follow up care thus improving outcomes.
Tele Rehabilitation; A peep into the Future
TR will eventually be integrated with Smart Homes in Smart Cities. Functional monitoring with bed sensors, activity/motion sensors and gait monitors will be a reality. This will be followed by Creating a connected home with pressure-sensing floors, smart furniture and medical sensors. Assistive robots, power wheelchairs, prosthetic limb controls, Home Automation systems and AI Chatbot companion at Home will add value providing “smarter care”. This will include encouraging activities and contacting caregiver/children in emergencies. Staying @ Home, better known as aging in place will lead to better health outcomes.
Conclusion
Understanding who will use TR, how it will help achieve customized, well defined and changing goals is critical. Beneficiary’s goals alone matter. TR is only a tool to achieve them. The Health Care Provider using TR should get into the minds of the the end user. It should never be forgotten that for digital natives, an octogenarian is from another planet. “Customer delight” is not a cliché used as a marketing ploy. TR is not a solution searching for a problem. Nothing can stop an idea whose time has come. Covid has ensured that Telerehabilitation is here to stay.
The Key Note Address is available @ https://youtu.be/RNEIZqc3w5A
Telemedicine and Its Applications for the Common Man during COVID Pandemic – A three-day virtual online lecture series by ISIE Ahmedabad
Mr. Anil C. Mathur
Group Director (Retd.),Space Applications Centre, ISRO, Ahmedabad | MD, Indian Space Industries Exhibitors, Ahmedabad-Ghaziabad | Email: antrixudyog@gmail.com
In this era of digital world, technology is going to play a big role in establishing India as a superpower. Telemedicine is one such area. Telemedicine, also known as telehealth or e-medicine, is the remote delivery of health services, including examinations and consultations, on telecommunications infrastructure. Telemedicine is the practice of medicine using technology to deliver care remotely. A physician at one location uses a telecommunications infrastructure to provide care for a patient at a distant location. Telemedicine allows healthcare providers to evaluate, diagnose and treat patients without the need to meet in person. Patients can communicate with physicians from their homes using their own personal technology or by visiting a dedicated telehealth kiosk.
A three-day virtual online lecture series on the theme “Telemedicine and Its Applications for the Common Man during COVID Pandemic” was organized by Indian Space Industries Exhibitors (ISIE) Ahmedabad from 10 July 2021 to 12 July 2021. ISIE is a micro-venture established under Micro, Small and Medium Enterprises (MSME). This organization has been founded by Mr. Anil C. Mathur, retired group director, ISRO Ahmedabad and alumnus IIT Roorkee. From the very beginning, ISIE has encouraged the public especially scientists, students, science communicators to adopt science and technology applications in daily life.
The programme was virtually inaugurated on the Zoom stage by the Chief Guest Shri B. S. Bhatia, Former Director,DECU/ISRO, Ahmedabad. In the inaugural session, Mr. Bharat Mehta, Editor-in-Chief of the journal “Space Industry” published by ISIE, gave information about the activities of ISIE and repeated strongly, the goal of all the organizers to bring the activities and benefits of space science and technology to the common man of the country. The Chief Guest of the inaugural session Shri B. S. Bhatia expressed his thoughts on the importance of telemedicine for shaping the diverse possibilities of a futuristically developed world. Mr. Dinesh Kumar, Chairman Institute of Engineers Delhi State Centre, also addressed the participants in the inaugural session as a special guest.
In this virtual series of lectures, online addresses were given by eminent doctors, scientists, technical and industrial experts of the country in the sessions organized between 10 am IST to 4 pm IST on all three days. In this three-day virtual online lecture series, the experts tried to portray the future India’s telemedicine healthcare technology to capture the imagination of the audience, especially the students, by giving their address session wise as follows according to the schedule:
India’s Space programme and History of Telemedicine in India by Mr. A. K. Sangal, Retd. Group Director, DECU/ISRO and former President, Telemedicine Society of India; Telemedicine Society of India , its training activities and Relevance of Telemedicine in the Covid pandemic by Dr. Ashvini Goel, Retd. Colonel (Dr.) Indian Army, and Current President, Telemedicine Society of India; Applications of Telemedicine in Surgical care and Skill transfer by Dr. S. K. Mishra, Founder President, TSI and Senior surgeon and Dean at Sanjay Gandhi PGI, Lucknow; Telemedicine – Accessible and Affordable Healthcare for All by Dr. Sunil Shroff, President Telemedicine Society of India, Tamil Nadu Senior Consultant Urologist Madras Mission Hospital; Role of Videoconference in Telemedicine by Mr. Bijoy M. G., Managing Director, Unarv Telemedicine & Healthcare Services (P) ltd, and Secretary Kerala state chapter of Telemedicine Society of India; Tele-health activities during Covid-19 pandemic-Odisha Experience by Dr. B. N. Mohanty, Hon. Advisor to the Odisha Government and former president of Telemedicine Society of India; Merits, demerits and problems associated with Telemedicine Network and System by Dr. T. N. Ravishankar, Specialized family physician and currently Director Sudar Hospital; Applications and Usage of advanced Artificial Intelligence(AI) technology in Health Care by Dr. Masood Ikram Doctor turned entrepreneur and expert in applications of AI in the Healthcare industry; Telemedicine-During and after COVID pandemic by Dr. Sanjeev Mehta Senior pathologist, Ahmedabad and Member Telemedicine Society of India; ISRO’s Telemedicine Network by Mr. Arvind Tyagi Scientist/Engineer, DECU/ISRO, Ahmedabad; NavIC, Telemedicine and the COVID by Dr. M. R. Sivaraman Retired Scientist/Engineer ‘G’ and DPD, SAC/ISRO, Ahmedabad; Lessons from Covid-19 for Community enabling to counter infodemic by Mr. J. Venkataramaiah, Retd. Sci./Engr. ISRO. Alumni & Mentor, International Space University. Currently associated with PSF; Clinical Applications of Telemedicine by Dr. N. K. Agarwal Professor of Endocrinology and Nodal Officer of Regional Resource Centre of Telemedicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi; Block Chain in Healthcare by Dr. Bhagwant Singh Ratta Pediatric Surgeon/Urologist and former president Telemedicine Society of India; Continuing Medical Education through ISRO’s Telemedicine Network and Tele-consultations during Covid-19 by Dr. Maulesh Gadani, Medical Officer, SAC/ISRO, Ahmedabad; Telemedicine- What really works by Mr. Mayank Agarwal CEO, M/s Smart Square Tech., NOIDA; Televital Journey and Latest Trends in Telemedicine Technology Mr. Sateesh Bhatt Solution Architect, M/s Televital India Pvt. Ltd., Bangalore; Telemedicine and Privacy by Ms. Bagmisikha Puhan, Technology Lawyer and Privacy Practioner, EC member Telemedicine Society of India.
The concluding session of this lecture series on 12th July, was presided over by Dr. Velchamy, Founder ‘Krithin Foundation’, Trichy, Tamil Nadu. Dr. SK Mishra, former Head of the Department of Endocrine Surgery and Nodal Officer Telemedicine Program, S.G.P.G.I. Lucknow; Shri AK Sangal, Former Scientist SAC, ISRO, Ahmedabad; Shri Vikram Desai, Former Director DECU ISRO; Shri VK Jain, President BES Ahmedabad Chapter; Shri Anil C. Mathur, Managing Director, ISIE expressed their views while discussing the future roadmap of telemedicine through panel discussion.
On all three days of the lecture series, BES Ahmedabad Chapter President Shri VK Jain conducted the entire program with technical support from the team of Space Geeks led by the Founder Shri Chintamani Pai, Dr. Vaibhav Rawat and Shri Hari Tejas Iyer. At the end of the program Shri Amritanshu Vajpayee, Founder Coordinator, Ignited Minds VIPNET Club-Farrukhabad presented a formal vote of thanks and then the end of the three day virtual lecture series was announced by the organizers. Due to this unique effort of ISIE in the midst of the worldwide pandemic of COVID-19, this three-day virtual online lecture series can be considered as an effort to reach out to the masses through participating audiences belonging to different fields.
Broadcasters Engineering Society Ahmedabad Chapter, Space Education and Research Foundation, Space Geeks Mumbai, UL Space Club, IITR Alumni Association Ahmedabad, UOR77 Batch Foundation New Delhi, Space Education and Research Foundation Ahmedabad, Ignited Minds VIPNET Club -Farrukhabad were the collaborating organizations as knowledge partners and Sunrise India Samachar – New Delhi was associated as a media partner for the programme. Many serving and former scientists of ISRO as well as representatives of different collaborating institutions graced the occasion. The live broadcast of the event was arranged by the organizers on the YouTube channel of Indian Space Industries Exhibitors, viz., https://youtube.com/c/ISIEIndianSpaceIndustryExhibitors. The entire virtual lecture is available for public viewing on the channel above.
 |
 |
 |
 |
 |
 |
 |
 |
Medical Negligence in the Telemedicine Era
 Anay Shukla
Anay Shukla
Founding Partner, Arogya Legal – Health Laws Specialist Law Firm
Eshika Phadke
Associate, Arogya Legal – Health Laws Specialist Law Firm
In our previous articles, we discussed the legal considerations and compliances that must be followed to practice telemedicine in India. In this article, we are going to examine a less pleasant but equally important subject: how does a doctor protect themselves from allegations of medical negligence while practicing telemedicine?
It is important to first understand what medical negligence is. When a doctor-patient relationship is formed, a duty is cast upon the doctor to act and provide treatment to the patient as per the applicable standards of reasonable care. Any act (including a failure to act) by a doctor that is in a breach of the standard of care, which results in the patient being harmed, would constitute medical negligence.
Standard of reasonable care
The standard of reasonable care that is applicable to a doctor differs based on specialization, level of education and amount of experience, and is ascertained on the basis of what would be considered reasonable by a responsible body of professionals in that specialization for a doctor with ordinary skill.
For telemedicine, the jurisprudence around the “standard of reasonable care” is still in a stage of infancy in India, since telemedicine was only legitimized in March last year. The Telemedicine Practice Guidelines (“Guidelines”) make it clear that the professional and ethical norms that are applicable to in-person care are also applicable to telemedicine, bearing in mind the intrinsic limitations of telemedicine. So, while the principles of medical negligence for traditional consultations remain the same, they must be adapted to virtual consultations.
At a fundamental level, deviating from the practices laid out in the Guidelines would be considered a breach of standard of reasonable care, and if it results in harm to the patient would constitute medical negligence. Doctors should familiarize themselves with telemedicine guidelines for their specialty to get a clear understanding of what is recognized as the standard of reasonable care.
Documentation and Consent
Similar to in-person consultations, documentation is of utmost importance, not only because it is required under the law, but also because it serves as the doctor’s primary defense should a patient make allegations of negligence or deficiency in service in court.
While consent for the consultation is implied when the patient initiates the consultation, explicit consent must be sought in all other cases. For instance, if the patient’s caregiver or another healthcare professional initiates the session. In such cases, consent ought to be recorded. As a precautionary measure, doctors should also record if a patient refuses to act as per instructions, which may result in their condition worsening. In particular, if a doctor deems an in-clinic visit necessary but the patient refuses, the doctor should obtain, in writing, a declaration from the patient that he/she has been informed of the risks of proceeding via telemedicine and has been advised to visit a doctor’s clinic, but is electing to proceed with telemedicine.
Delay in seeking treatment
The most likely scenario that would result in allegations of negligence is if a doctor does not recommend that a patient see a doctor in-clinic, when it is evident that it is required or fails to communicate the urgency with which the patient ought to seek in-person care. If the patient’s condition deteriorates as a result of the delay in receiving the treatment that they require, the doctor with whom the patient did a teleconsultation with will likely be held for negligence.
Incorrect mode of teleconsultation
The Guidelines recognise video, audio, real-time text and asynchronous interactions between a doctor and patient as telemedicine. While a doctor is at liberty to select which mode to adopt, it is essential that they act prudently while doing so and ensure that the mode allows them obtain all the information required to take a decision. If required, it is perfectly acceptable to switch to another mode. If failure to adopt the most appropriate mode results in a failure to diagnose or misdiagnosis or incorrect treatment, it would likely be considered negligence on the doctor’s part.
Prescriptions
It has been held that prescribing a drug without following the due process to arrive at a diagnosis amounts to (criminal) medical negligence. Doctors must be especially wary of this before prescribing a course of treatment via telemedicine, and must ensure that they have gathered all the relevant information (which may include shifting to a different mode of teleconsultation or requesting the patient to visit a doctor for a physical examination, and ordering diagnostic tests) prior to writing the prescription. Doctors should also ensure that they strictly adhere to the limitations specified in the Guidelines in relation to drugs that may be prescribed via telemedicine.
REFERENCES
1.Indian Medical Council (Professional conduct, Etiquette and Ethics) Regulations, 2002.
2.Telemedicine Practice Guidelines
3.Deepa Sanjeev Pawarskar & Anr. v. The State of Maharashtra (Bombay High Court)
Birth of Tele-Radiology (History and Evolution of Telemedicine –9th Milestone)
 Dr. Sunil Shroff, MS, FRCS, Dip. Urol (Lond.)
Dr. Sunil Shroff, MS, FRCS, Dip. Urol (Lond.)
President, Tamil Nadu Telemedicine Society of India,
Editor, www.medindia.net,
Consultant Urologist & Transplant Surgeon, Madras Medical Mission Hospital, Chennai, India (shroffmed@gmail.com).
Tele-radiology has been an integral part of development and advancement of telemedicine. The advantage has been that it can use asynchronous technology of store and forward to transmit the heavy images to another location for reporting. Important early milestones I the development of Tele-Radiology have included –
In 1929 – Dental x-rays were transmitted with the help of telegraph to a distant location
In 1959 – Canadian radiologist reported diagnostic consultations based on fluoroscopy images transmitted by coaxial cable
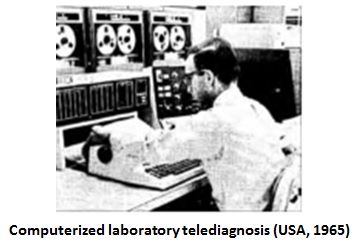
Radiologist Joseph Gershon-Cohen and inventor Austin Cooley spent 2 years testing a system invented by Cooley to connect Chester County Hospital to Philadelphia, PA, 28 miles away through wire and radio circuits. The early process was described by Bashshur RL as follows:
‘Primitive by modern standards, the equipment consisted of a glass drum with a clamp on top to attach the film while the drum rotated at a uniform speed of 180rpm. A beam of light illuminated tiny elemental areas of the film and picked up by a photo cell inside the cylinder and connected with a preamplifier to produce the full picture. The image was passed through an output amplifier before connecting it to a telephone line or radio transmitter.’
The two authors eloquently described the essence of their invention: “Consultation between the roentgenologist and surgeon, twenty-eight miles apart, took place over the same telephone circuit, with no more delay than a similar consultation would entail with the surgeon and roentgenologist present together in the hospital.”
It was in 1993 that the American College of Radiology (ACR) and the National Electrical Manufacturers Association (NEMA) brought minimum standards for medical images and metadata, with respect to handling, storing, printing, and transmitting images and other medical record information. This was called ‘Digital Imaging and Communications in Medicine’ (DICOM). DICOM is today an internationally accepted standard for medical images and applies to a number of key aspects of the digital radiology enterprise. It also has standards for file format and network communications.
In India, the first successful use of teleradiology transmission was done in 1996 was done from Jankharia Imaging in Mumbai where image was transferred to the homes of the individual doctors for reporting emergency CT scans.
Reference
1.Sending dental X-rays by telegraph. Dent Radiogr Photogr. 1929;2:16. monitoring (Davis et al., 1961)
2.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5107673/
3.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2747412/
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI
To know more about the Telemedicine Foundation Course click on the link below:
https://tsi.org.in/courses/
Telemedicine – News from India & Abroad
India
Artificial Intelligence (AI) Unfolds the New Dimension of Social Development
‘Artificial Intelligence (AI) proves as an inevitable tool in achieving Sustainable Development Goals (SDGs – 17 interlinked global goals for a better future). A global virtual event organized by Amrita Vishwa Vidyapeethamprovided excellent and up-to-date research for all AI enthusiasts from the industry, academicians, and students to realize the importance of AI in all fields. ’….. Read More
International
Recent Improvements In Pharmaceutical Sector
AI and big data/analytics are identified by healthcare industry professionals as the top technologies that will transform pharmaceutical drug discovery and development processes, according to a survey by GlobalData, a leading data and analytics company……….. Read More
Machine Learning-powered Imaging Helps Diagnose Thyroid Cancer
A new non-invasive method to distinguish thyroid nodules from cancer by combining photoacoustic (PA) and ultrasound image technology with artificial intelligence has been devised by scientists…. Read More
AI-powered emotion analysis technology to help diagnose mental health conditions in seniors in Singapore
Through video calls, Opsis Emotion AI’s software will be used by counsellers to help diagnose mental health conditions such as anxiety, stress and depression. Emotional analysis technology developed by software solutions provider Opsis Emotion AI will be piloted over the next two years in a programme targeting more than 4,300 seniors in Singapore.….. Read More
New Revelation About Brain Activity During Sleep
Using an artificial intelligence approach, scientists at the University of Geneva (UNIGE), Switzerland explained the brain activity during sleep. They provided strange evidence that sorting out of things during the day time takes place during deep sleep by combining functional magnetic resonance imaging (fMRI) and electroencephalography (EEG).….. Read More
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
|
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- www.medindia.net