Click Here to Download PDF Version

Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
| What is New?
The Omicron wave is yet another reminder that the uncertainty of this pandemic continues to haunt us but now with tele-health ecosystem getting established, the challenges are less in managing and providing care. The importance of telemedicine for Indian healthcare sector was further stressed by our Union Minister Dr. Jitendra Singh says and he said ‘Tele-medicine Technology is going to be the Main Pillar of India’s Future Health Care System.’ The Consultation Paper on Proposed Health Data Retention Policy that opened out the discussion and asked for suggestions and Recommendations last month was an interesting exercise. We from Tamil Nadu & NCR Chapter of Telemedicine Society of India sent our recommendations to the National Health Authority. It makes interesting reading hence we have enclosed it in the newsletter. Thank You |
Union Minister Dr Jitendra Singh says, Tele-medicine technology is going to be the main pillar of India’s future health care system
Highlights:
- Dr Jitendra Singh launches Tele-digital Health Pilot Program at BHU, Varanasi
- The project starting in three districts of Varanasi, Gorakhpur and Kamjong in Manipur will cover 60,000 patients in the initial phase
- Minister says, project to generate Electronic Health Record (EHR) for Indian population
- Tele-medicine could save India between 4-5 billion US dollars every year: Dr Jitendra Singh
Union Minister of State (Independent Charge) Science & Technology; Minister of State (Independent Charge) Earth Sciences; MoS PMO, Personnel, Public Grievances, Pensions, Atomic Energy and Space, Dr Jitendra Singh today said that Tele-medicine technology is going to be the main pillar of India’s future health care system.
Launching the Tele-Digital Healthcare Pilot Program at BHU, Varanasi, Dr Jitendra Singh said, innovative healthcare solutions like Tele-medicine could save India between 4-5 billion US dollars every year and replace half of in-person outpatient consultations. The Minister said that Prime Minister Narendra Modi’s Digital Health Mission is the next frontier to ensure healthcare delivery is accessible, available, and affordable to all, particularly the poor living in rural and inaccessible terrain. He said, Telemedicine in the country has proven to be cost effective by about 30% less than equivalent in-person visits.

Dr Jitendra Singh said that though Telemedicine technology was in vogue for quite some time in the country, but it got a fillip in post-COVID era and in the wake of PM Modi’s push to Digital Health Ecosystem in India.
Referring to Drone delivery of vaccines in some parts of India, the Minister said, with rapid advancement in technology, Robotic Surgery will also become a reality very soon and future doctors will increasing don the mettle of Tele-Doctors.
Pointing out to very low doctor-patient ratio in India that is about one per 1,457 Indian citizens, Dr Jitendra Singh said, Tele-medicine is no longer an option but a necessity. He said, about 65 percent of India’s population that lives in rural villages, where the doctor-patient ratio is as low as one doctor per 25,000 citizens and therefore they must get best of medical advice from doctors based in towns and metropolitan cities. He said, Telemedicine will not only help the patients save their time and money, but also the doctors who can quickly assist their patients over a call for the same and actively engage in promptly treating patients with major ailments.

Dr Jitendra Singh said, the project starting in three districts of Varanasi, Gorakhpur and Kamjong in Manipur will cover 60,000 patients in the initial phase and it will be scaled up gradually to cover the entire country in the coming years. Technology Information, Forecasting and Assessment Council (TIFAC), an autonomous body of Department of Science and Technology at the Centre has designed a pilot Tele-diagnostics project in collaboration with IIT Madras-Pravartak Foundation Technologies & CDAC Mohali. This will also generate Electronic Health Record (EHR) for Indian population.
The Minister said, the project is a scalable pilot PLUG and PLAY model oriented to provide quality medical care to underprivileged women and children living in remote areas at affordable costs. The key activities include examination of the patients: women/ children with wearable devices, transferring the health data record through the e-sanjeevani cloud to a pool of doctors for analysis, and concurrently for development of EHR. The parameters that would be analysed include: ECG, Heart Rate, Blood Pressure, Lipid Profile, Haemoglobin & Foetal Doppler.
It may be recalled that Dr Jitendra Singh has established tele-consultation facility in his Lok Sabha Constituency of Udhampur-Kathua-Doda from his MP-LAD Fund, in the District Hospital Udhampur with all the Panchayats connected with it and it is being monitored on a regular basis.
Dr Jitendra Singh said that Prime Minister Narendra Modi has given very high priority to the Health Sector and this year’s budget increased the spending on healthcare by 137%, which is in line with industry expectations of 2.5%-3% of the GDP. The Minister informed that India will spend Rs 2.23 lakh crore on healthcare this fiscal including Rs 35,000 crore on Covid-19 vaccines.
The Minister said that various health care schemes launched by Modi Government such as PM Ayushman Bharat Health Infrastructure Mission, Ayushman Bharat Jan ArogyaYojana, Ayushman Health and Wellness Centres, Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP) and Ayushman Bharat Digital Mission have made healthcare facilities accessible and affordable to millions of poor people in the country. Read More
Consultation Paper on Proposed Health Data Retention Policy
Recommendations from Tamil Nadu Chapter & NCR Chapter of Telemedicine Society of India hat was sent to the Joint Director (Coordination),National Health Authority Delhi
2.4 Key Issues for Consultation
1. Whether there is a need for a Health Data Retention Policy and will Indian healthcare ecosystem benefit from such a Universal Data Retention Policy and what should be the key elements of this policy?
Ans. Yes this is indeed required with advent of digital health and to make it uniform. Though we have had a late start in India, however we can learn from experience of other countries and avoid their errors
The key elements of the policy should be as follows –
Structure
- Formulate an independent body with reps from govt and non-govt organisations
- Invite a few stakeholders from some leading countries on the board Focus
- Interoperability of such data
- Define data types and subtypes and give each weightage for storage
- Broadly define acute care vs chronic care – more so with the increasing burden of NCDs. There is a need to store chronic care data for longer
2. How should the guiding principle of this policy be determined for the benefit of stakeholders and ease of adoption by varying sizes of entities deciding to opt in for ABDM?
- Keep the policy flexible with a review every five years,
- Storage should be in digital format,
- Irrespective of size of entity storage time should be the same especially if it means data sharing
3.2 Key Issues for Consultation
1. As per Option 1, it has been proposed that the policy would be applicable to all healthcare entities from health data retention perspective. As per Option 2, the policy will be applicable only to entities participating in ABDM? Which would be a better option for the scope of the health data retention policy?
Ans. This has to be work in evolution. Ideally option 2 should be possible but this can become a nonstarter considering the complexity of the current healthcare infrastructure and digitations and lack of standards
Our recommendation the policy will be applicable only to entities participating in ABDM to start with an objective to integrate other entities in future.
As GoI is going to be both the provider and the payer ( through its universal health insurance schemes) it will not be too difficult to set standards and have a uniform system.
After the initial learnings it can recommend other entities too join.
However an option can be provided to all entities to join without making it compulsory
2. How such a policy should be implemented given limitations in terms of infrastructure, capability, and sufficient understanding of health data in the healthcare ecosystem?
This will take time but then following would be required-
- Regular seminars and educating healthcare professionals and managers
- Setting minimum standards requirement and making this a requirement for accreditation for health insurance claims, NABH and NABL
3. As ABDM has a provision for opt-out, in such a scenario what may be the possible implications from the perspective of health data retention?
Ans. This has been answered in the first question. A flexible approach would help stakeholders understand and appreciate the importance of data harmonisation and data retention. It would help avoid fear psychosis, would give time and feedback of what is implemented and make changes in the policies.
Having the payers on the side of the GoI would also help entities to fall in line.
However, where ever the GoI is a stakeholder as a payer and provider – it should be made compulsory and no opt out option should be provided.
4.8 Key Issues for Consultation
This is the most important chapter of the current document. What must remember is that so far the hospitals have followed a physical format of preservation of data. While this has certain advantages in a hospital setting for a follow up system for medical professionals but it adds costs for physical storage, retrieval, classification and maintenance.
This has resulted in many hospitals not having a medical records section at all resulting in patients carrying their medical file from hospital/doctor to another hospital/doctor.
The digitation of records help the whole ecosystem and creates efficiency in the it.
1. Should a blanket retention duration be adopted for all health records in India or different schedules be defined as per a classification? Which is a better approach of retention?
Ans. If blanket retention is followed it would avoid much confusion and discussion.
The number of years for data retention are random and there are no studies that these periods make any sense in the context of data retrieval or other requirements and these are based to lessen the physical storage burden. However, with digitisation of data and the cost of the same coming down, a rethink is required as this is a new paradigm we are addressing and has no comparison to the physical world.
2. How granular should data classification be? Is more granularity required beyond that presented in the sections above? Addressing this aspect of the Health Data Retention Policy would help assess whether minimalist data classification – pertaining only to inpatients and outpatients – would suffice the purpose of health data retention. A minimalist data classification would have both advantages and disadvantages. Please suggest your view in this regard.
And 3. How in your view will a detailed granular data classification enable a better health data retention? Please suggest your view on the classification of health record types as proposed above or if any further granularity is necessary and what are the overarching benefits for different stakeholders?
Ans. Most health data are interlinked from point of patient care and really subclassifying again applies better when there is a physical need of storage of such data.
A new paradigm of data classification will emerge in the digital world. It may be defined as a health condition being cured or not cured. Being acute and cured or acute and not cured or chronic and cured or chronic and not cured.
Again, if blanket retention is followed granularity of data would have not much meaning
4. What should be the ideal duration for these different health data types?
Ans. Different countries follow different timelines and this is random depending on investment in medical record section.
It is generally recommended that the Personal health record should be available for lifetime hence why should other data retention be looked at differently.
UK follows 20 to 25 years. We currently feel this should be the minimum time of retention with a recommendation for it to be ideally for lifetime.
We need to look ahead and serve the new generation borne in the digital age. For a child born today, 10 years of data retention would be meaningless. For someone with chronic care one can’t delete data that goes beyond 10 years.
At this stage as said earlier, the minimum period should be defined as not less than 20 years and recommended for lifetime. A review should be possible in time to come. 10 years is too short a time.
5. While ABDM proposes that all entities opting to join NDHE must be able to retain health data in electronic format, and other entities of the healthcare ecosystem may consider physical or original formats, what options should be made allowable as part of the policy being proposed? Health data records can be only digital, only physical, or combination in any hospital. Accordingly, the question arises whether all the above considerations should fall under one policy or under separate/independent policies?
Ans. Digital format should be compulsory and physical should be optional. A uniform policy would cause less confusion and also be a trigger for the much required change.
6. Should there be a provision for extension of duration or retention of health data under the policy being proposed? What considerations should be made in defining the guidelines, allowing for such an extension?
Ans. Keeping it flexible is the key as time would be required for change. However, at the same time to quicken the process Incentives or a reward system could be created to hospitals, entities, states, cities etc that adopt and implement the change.
In fact, as a starting point all smart cities policies should have this policy as one of the pre-requisites.
7. Who shall have the apex authority to oversee and implement health data retention? Which entity as part of the ecosystem should be rolling out this policy at the macro-level?
Ans. Initially the National Digital Health Authority should be in charge, however creating an independent body with key stakeholders would be ideal under the National Digital Health Authority.
8. How can smaller clinics or centres, both public and private, build capability in a timely and cost-efficient manner to take responsibility of data retention for long time periods?
Ans. The health insurance in the country already has certain requirements and many smaller clinics are slowly adopting some of these requirements. Most will eventually have to fall inline or the larger good.
Hospitals with less than say 25 beds maybe given a longer gestation period for adoption.
9. How can business continuity be ensured in case of fall of the establishment, platform or service providers?
Ans. This is going ot be challenge and requires further deliberation.
In case of closure of an establishment all the data should be transferred to a central repository which can be state or central driven and a mechanism would need to be devised.
Questions to be answered –
- Format of such a body
- If the data is in physical format who would bear the cost of digitisation
- Method of usage of such data
5.5 Key Issues for Consultation
1. Will the governance model as per Health Data Management Policy be sufficient for the retention policy?
Ans. There needs to be audit system by third party that needs to be built in to ensure trust, compliance and accountability
2. How will the policy regulation be enforced and what should be the structure across relevant entities responsible for retaining the health data?
Ans. This would require to be implemented as addendum to many regulations.
Some of these would need to be part of the regulatory structure of PDP Bill on data protection after it is passed by the GoI
3. How should the implementation of the policy be done in case the policy is made applicable for the ecosystem beyond ABDM?
& 4. Is there an alternative model or policy approach which could be considered?
Implementation of the policy will happen if it becomes part of a regulatory requirement.
A start needs to be made and it needs to evolve and change from time to time. There are no perfect policies or perfect implantation and one cannot have all the answers to various questions that crop up.
A Unique Blended Mental Health Support Delivery Model
Smriti Joshi, MBPsS, M.phil in Clinical Psychology
Advanced Certified Telebehavioral Health Professional (www.telehealth.org) | Lead Psychologist & Member Board of Directors, Wysa
In-person mental health support is not replaceable yet it cannot scale enough to address this rapidly increasing need to provide mental health support to this growing public mental health support crisis. (AI)-enabled, empathetic, and evidence-driven conversational agents are now being considered a way to rapidly scale mental health support provision, augmenting existing mental health services. Wysa is one of the world’s leading solutions in this space, with 4 million users served, who have had 485 million conversations in 65 countries.
Wysa was founded in 2016, and I am part of the 5 member founding team.
A. Wysa Introduction & Background
Wysa ‘s service model can be best imagined as a unique 3-layer ‘pyramid of care’, based on an anonymous, text-based app interface that can create custom care pathways. App users get help through –
(1) an emotionally-intelligent AI-CBT delivering chatbot providing 24X7 support,
(2) a library of evidence-based self-help tools and techniques to help build resilience.
(3) online therapy with professional clinical and counselling psychologists.
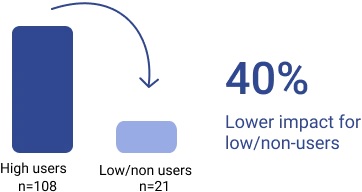
The model is affordable (cost of triage can be 90% lower), scalable (It can support a 4 million user base with a 70 people team), and flexible to integrate with existing service ecosystems; so it is very suitable for early stage intervention, and support at a population level.
The AI is built inhouse, and tuned for emotional intelligence, delivering evidence-based AI-driven Cognitive Behavior therapy (AI-CBT). Wysa allows for free text input which makes the conversation empathetic allowing for a richer user experience. Wysa’s 100+ NLP models, built on 485 million+ conversations, make its ‘listening’ ability unique and the best in the world today. This AI meets global Clinical Safety standards, are ISO certified, and is explainable using non-generative models that can be audited for clinical safety.
B. Global Leadership
Wysa is a global leader in conversational AI for behavioral health and has already helped improve mental health care for over 4 million individuals across 65 countries. It is the preferred digital behavioral health partner for organizations like Accenture, Aetna, Travelers, and the National Health Service (NHS) in the UK, and the Ministry of Health in Singapore.
Wysa is rated #1 at 93% by ORCHA, the NHS digital app evaluation agency – the highest across all categories – including a 100% on clinical assurance.

It has recently won the NHS NIHR AI Award, aims to accelerate the testing and evaluation of AI technologies in the NHS so patients can benefit from faster and more personalized diagnosis and greater efficiency in screening services.
- NHS Featured App for Covid: link
- NHS ORCHA Best App in Health & Care (ORCHA is the NHS digital health solution evaluation agency): link
- Forbes Top 5 Innovations in Mental Health 2020: link
- Google Play Best App 2020
- CB Insights 25 Technologies Changing the Post-covid World: link
- Cincinnati Children’s Hospital (US) Recommended solution for Covid management: link
- ORCHA 10 Best Apps to Manage Long Covid: link
Wysa’s efficacy for managing depression has been established through a peer-reviewed study published in JMIR, the world’s top e-health journal. We are currently running clinical trials with Harvard Medical School, Columbia, Cambridge, Washington University and the NIHR in the UK: 10 other research papers are underway, and will be published in 2022.
C. My Role & Contributions
The last 6 years of working at Wysa have been the most productive and fulfilling years of my career as there has been immense learning around how AI and machine learning can make healthcare more accessible and scalable and bridge the existing gap in service provision due to various challenges.
Apart from being part of Wysa’s founding team and serving on the Board of Directors, I have set up a 30-people clinical and therapist team that supports clients from India and 30 other countries using Text based and Audio-video counselling and psychotherapy – starting in India, we now have clinical team members in the US and UK. In addition to clinical inputs for product design for our AI platform, the team has also completed more than 10,000 therapy sessions in the past 3 years with a 95% client approval rating.
In addition, I have been the company’s senior representative at Swasth Alliance, an public-private partnership between the Ministry of Health & Family Welfare, Govt of India, and a consortium of startups in the Indian ecosystem coming together to serve the country during Covid. I am also part of the leadership team driving Wysa’s response to the mental health challenge brought upon by India’s third Covid wave, through a partnership with ACT Grants (a multiparty donor consortium) and the Govt of India.
The burden of care on health care professionals is immense. While setting up a team for remote delivery services, especially during the recent covid-19 waves, where psycho-therapy providers themselves were struggling with covid-19 related concerns, I developed a keen interest in an area often neglected by practitioners themselves- compassion fatigue and burnout in health care providers.
Ensuring my team’s well being and building team resilience became my key focus and I ensured that this work was carried out via an action based research effort at Wysa.
We are creating new models of tele-therapy that combine human support with AI-led CBT, that are cutting-edge and unique and our unique culture, ethos and spirit of service are being recognised in clinical and practitioner communities within tele-therapy globally. I have been invited to offer mentoring and support to aspiring psychologists from across the world via this https://www.therapistsintech.com/ to assist them in their phase of transition from making a shift from in person clinical practice or academia to delivering services via online modalities and also helping platforms build resilient remote service delivery teams, especially in the wake of covid-19. These efforts were acknowledged by this international platform and I was awarded with “The outstanding mentor in tech award for 2021”.

https://wysabuddy.app.link/dwwysa – Download Wysa Link
 A model for sustainable, partnership-based telehealth services in rural India: An early process evaluation from Tuver village, Gujarat
A model for sustainable, partnership-based telehealth services in rural India: An early process evaluation from Tuver village, Gujarat
Shoba Ramanadhan 1, Krishnan Ganapathy 2, Lovakanth Nukala 2, Subramaniya Rajagopalan 3, John C Camillus 4
Prof. Krishnan Ganapathy
Past President, Telemedicine Society of India & Neurological Society of India | Hon Distinguished Professor The Tamilnadu Dr. MGR Medical University | Emeritus Professor, National Academy of Medical Sciences | Formerly Adjunct Professor IIT Madras & Anna University | Director Apollo Telemedicine Networking Foundation & Apollo Tele Health Services | URL: www.kganapathy.in
Abstract
Background: Telehealth can improve access to high-quality healthcare for rural populations in India. However, rural communities often have other needs, such as sanitation or employment, to benefit fully from telehealth offerings, highlighting a need for systems-level solutions. A Business of Humanity approach argues that innovative solutions to wicked problems like these require strategic decision-making that attends to a) humaneness, e.g., equity and safety and b) humankind, or the needs and potential of large and growing markets comprised of marginalized and low-income individuals. The approach is expected to improve economic performance and long-term value creation for partners, thus supporting sustainability.
Methods: A demonstration project was conducted in Tuver, a rural and tribal village in Gujarat, India. The project included seven components: a partnership that emphasized power-sharing and complementary contributions; telehealth services; health promotion; digital services; power infrastructure; water and sanitation; and agribusiness. Core partners included the academic partner, local village leadership, a local development foundation, a telehealth provider, and a design-build contractor. This early process evaluation relies on administrative data, field notes, and project documentation and was analyzed using a case study approach.
Results: Findings highlight the importance of taking a systems perspective and engaging inter-sectoral partners through alignment of values and goals. Additionally, the creation of a synergistic, health-promoting ecosystem offers potential to support telehealth services in the long-term. At the same time, engaging rural, tribal communities in the use of technological advances posed a challenge, though local staff and intermediaries were effective in bridging disconnects.
Conclusion: Overall, this early process evaluation highlights the promise and challenges of using a Business of Humanity approach for coordinated, sustainable community-level action to improve the health and well-being of marginalized communities.
Publish or Perish
The Oxford Dictionary of Phrase and Fable, describes ‘publish or perish’ as an attitude or practice existing within academic institutions, whereby researchers are put under pressure to produce journal publications to retain their positions or to be deemed successful, The phrase is attributed to Coolidge who enunciated this theory in 1932. Successful publications draw attention to scholars and their sponsoring institutions. This , helps getting funds for research projects. However the pressure to publish also causes poor work being submitted to academic journals.
Publications in Telehealth have increased exponentially in the last 2 years. The author personally reviews at least one article a week from several international journals. Journals are measured by their impact factor (IF), which is the average number of citations per article published in that journal. Not many Indian journals have an impact index of even more than 2.5 .Neurology India for example has an IF of 2.7 . New England Journal of Medicine has an IF of 92 !! What is an author’s impact ?. This is traditionally measured using the number of citations a single article has received. Today this information can be obtained in real time. The impact of a publication can also be determined by the number of times a free access article has been downloaded.
The author’s first paper in a Pubmed indexed journal was as an MBBS student in 1972. https://pubmed.ncbi.nlm.nih.gov/4402191/. Since then one book has been edited, 20 chapters contributed and 79 papers published in indexed journals. Most of the 30 odd papers dealing with telehealth have been downloaded in large numbers. An article “ Distribution of neurologists and neurosurgeons in India and its relevance to Telemedicine ” https://www.neurologyindia.com/articleStatistics.asp?issn=0028-3886;year=2015;volume=63;issue=2;spage=142;epage=154;aulast=Ganapathy;aid=ni_2015_63_2_142_156274 has been downloaded 17,500 times and also often cited.
Publishing a paper in a well known journal is time consuming and labor intensive. In academic institutions a good library, secretarial help and residents are available to help the faculty to put together a paper. As mentioned earlier it is part of their job profile and is essential for survival. Interestingly more services in various aspects of telehealth are offered in the private sector. Here the story is different. In large private institutions a P&L driving CEO has concerns, and rightfully so, in making available “confidential” data in the public domain. Top journals insist on full access to nitty gritty. There is a conflict of interests. Paper publication takes a back seat. HR are dedicated to managing the operations. They generally do not have a Paper publishing background. Not being a part of their KPI it is extremely difficult to make them do extra work.
Publishing papers in national / international journals in the field of Telemedicine do have a RoI. Unfortunately this takes considerable time. It is not a low hanging fruit. From a purely personal growth perspective, every time one writes a paper, one becomes a little more knowledgeable. Literature review ensures that we are up to date. Defining the problem, spelling out exact aims and objectives, documenting observations , extrapolating inferences, writing a discussion and making conclusions when repeatedly done becomes part of one’s DNA. Writing an article makes one see the Big Picture. Getting an article accepted for publication is an art and a science. : https://www.neurologyindia.com/text.asp?2021/69/6/1547/333463. Adopting a scientific approach means more business !
India is indeed a paradox. In terms of numbers we probably provide more teleconsultations every single day than most countries on this planet. It is often stated that the sheer volume of work prevents us from meticulous documentation and follow up which is the sine qua non of doing any impact study. Interestingly even politicians and administrators want hard core scientific evidence that our remote intervention is cost effective resulting in significant difference in the ultimate health care outcome. The only way to get this evidence is to plan a paper for the NEJM and be patient for 3 years !! A prospective multi institutional well designed and funded study resulting in multiple papers alone will enable India to take a leadership role in the comity of nations. Improbable Yes. Impossible No. Do hope the Next Generation will take this seriously and not treat it as the rumblings of a septuagenarian. 22 years after the birth of Telehealth in India we should no longer follow high standards. We must set them. We should not be talking of achieving world class. The world should talk about achieving India class. We have the potential to bring out at least 40 papers every year in journals with an IF of > 2.5 . Doing qood quality work alone is not enough. The world should know about it !!
Handling Sensitive Situations through Telemedicine
Anay Shukla
Founding Partner, Arogya Legal – Health Laws Specialist Law Firm
Eshika Phadke
Associate, Arogya Legal – Health Laws Specialist Law Firm
The legalisation of telemedicine has been a boon for access to healthcare. However, the increased reliance on telemedicine has also been accompanied by unintended consequences: doctors may receive requests during consultations that are of a risky or highly sensitive nature, that they may not be comfortable handling.
For instance, a doctor may be consulted by a patient for a matter that requires an in-person examination, or it may be that the medication that the patient requires for their condition cannot be prescribed through telemedicine, but the patient refuses to visit a clinic or hospital and insists on receiving treatment through a teleconsultation only. In such a case, the doctor must inform the patient that a diagnosis cannot be arrived at or treatment cannot be commenced through a teleconsultation, and should meticulously record the patient’s refusal to seek a physical consultation. The doctor should inform them of the risks of not seeking proper treatment, and should record that the patient has been informed of the risks and is still refusing to seek proper treatment. Essentially, the doctor should capture that the patient was fully informed of the situation, and that he/she acted against medical advice.
In more extreme situations, a doctor may be consulted in an emergency situation where the patient requires urgent care. The doctor should advise the patient or caller to call an ambulance or rush to a hospital immediately. If required, the doctor may also inform the caller of the first aid measures that must be carried out.
There may be situation wherein a patient is verbally abusive or behaves inappropriately, perhaps even to an extent where the doctor feels uncomfortable or at risk. In such a situation, the doctor may advise the patient to consult with another doctor, end the consultation, and record his/her reasons for doing so. Depending on the severity, the doctor may also file a complaint with the police. If the doctor is consulting through a telemedicine service provider, he/she should also inform the management so that they can take appropriate actions.
If a patient is incoherent and appears to be either of unsound mind or inebriated, the doctor should ascertain whether there is a caregiver or trusted person whom the doctor may speak to for clarity and to give further instructions to. Doctors should exercise great caution while administering advice to a person who does not appear to be lucid.
A patient may display suicidal tendencies or even outrightly express that they intend to hurt either themselves or another person. In such situation, as with regular consultations, the doctor must promptly inform the authorities. Similarly, if the patient confides in the doctor that he/she is the victim of abuse or has been assaulted, the doctor should consider whether the authorities ought to be notified. Note that, to the extent that it is practical, guidelines for medicolegal cases should be adhered to for cases that are of a medicolegal nature.
Such situations are not specific to telemedicine, and may also occur with in-person consultations. Doctors should ensure that they apply at least the same level of prudence and professional judgment for remote consultations, and should ensure that they maintain meticulous records of such interactions (including any complaints made to authorities in relation to such interactions). Wherever possible, they should attempt to ensure that the records also reflect that the patient was made aware of the situation, and the patient concurs with what is being recorded in the doctor’s notes.
Telemedicine – News from India & Abroad
New Device Helps Measure Blood Pressure and Other Vitals
New ‘finger clip’ device has been designed to measure and monitor blood pressure consintuously, reveals a new study.Monitoring a person’s blood pressure on a regular basis can help health care professionals with early detection of various health problems such as high blood pressure…..Readmore
Artificial Intelligence (AI) Helps Improve Patient and Doctor Communication
Understanding between a patient with low health literacy and doctors can be improved with the help of artificial intelligence (AI) as per a study at the University of California – San Francisco, published in Science Advances.The study team performed a computer analysis of 250,000 … Read More
Click here to Become a Member of Telemedicine Society of India
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
|
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net



