
Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter. |
The December issue of TN-TSI Newsletter is dedicated to TELEMEDICON2020
![]()
TELEMEDICON2020 – Highlights
‘From the Fringes to the Mainstream’

Dr.Sunil Shroff, Organising Secretary, TELEMEDICON2020
The 16th International Annual Conference of ‘Telemedicine Society of India’ (TELEMEDICON2020) was held virtually from the 18th December to 20th December, 2020. This was the first International level Tele-Health conference after the notification of ‘Telemedicine Practice Guidelines’ by the Govt. of India in this ongoing COVID pandemic.
Since Lucknow could not do a physical conference due to the ongoing pandemic, it was decided to go ahead with a virtual meeting and Tamil Nadu chapter along with four other TSI state chapters which included Delhi-NCR, Rajasthan, Maharashtra and Karnataka took up the responsibility and mandate to conduct this web conference. The time was very short and the task herculean,however due to cooperation from many this was accomplished successfully.
As an organising body we created various committees and the scientificcommittee met over six times to put forward a compelling program with an objective to capture the essence of the theme of the conference on how Telemedicine in India had moved from the very ‘Fringes to the Mainstream’ within a very short span of few months.
![]()
![]()
The Conference was graced with the stellar presence of Hon’ble Justice of Supreme Court ShripathiRavindra Bhat, Mr. AnupWadhawan, IAS, Secretary, Ministry ofCommerce and Industry; Dr. Vinod KPaul, Member, NITI AAYOG; Dr Dharmendra Singh Gangwar, IAS, Addl. Secy. & Fin Advisor Min of Health &Family Welfare; Mr. Lav Agarwal, IAS, Jt. Secy., Ministry of Health and Family Welfare; Dr.SoumyaSwaminathan, Chief Scientist, WHO, Lt Gen ( Dr) MadhuriKanitkar;Ms. VandanaGurnani, Addl. Secy. and Mission Director of the national Health Mission at theMinistry of Health and Family Welfare, Government of India; Mr. Frank Lievens ( Belgium),ISfTeH Executive Secretary (Switzerland) and Dr.Prof. Thais Russomano (UK),Space Physiology, Aviation Medicine, Telemedicine & Digital Health Co-Founder & CEO, InnovaSpace UKamongst others.
The presidential Oration was delivered by President Maj Gen (Dr) AK Singh (Retd.)and he spoke about his experience over the years in the Telehealth space in India.
The chief guest for the inauguration Dr. Vinod KPaul, Member, NITI AAYOG, spoke truly from his heart and gave a message of hope and spoke about the responsibility that had been bestowed on the medical fraternity for creating a tele-health ecosystem as a new enabler for providing affordable access to universal healthcare in India.
| Chief Guest for Inauguration function of TELEMEDICON2020Dr. Vinod KPaul, Member, NITI AAYOG delivered his chief guest address. | Dr Dharmendra Singh Gangwar, IAS, Addl. Secy. & Fin Advisor Min of Health & Family Welfare delivering the Keynote address. He inaugurated the Virtual Exhibition for TELEMEDICON2020 |
| Presidential Oration by Maj Gen (Dr) AK Singh (Retd.) | Dr. B.N Gangadhara, Chairman, Ethics & Medical Registration Board, National Medical Commission gave his keynote address on ‘Emerging Ethical challenges in Digital Health’ |
|
Mr. Lav Agarwal, IAS, Jt. Secy., Ministry of Health and Family Welfare delivering his keynote address at the Valedictory Function on the Way Forward for Telehealth. He also released the Telemedicine Practice Guidelines FAQ’s for Medical Practitioners from TSI.
|
Synopsis of Presidential address

Maj Gen Dr. A K Singh (Retd.)
President
In his own words –
The year 2020 has been a very tough year for all of us but for Telemedicine Society of India it has been a year where the TSI has trained over 15,000 Doctors after the Telemedicine Practice guidelines were issued by the board of governors (MCI).
The training team led by Dr Sunil Shroff curated a very comprehensive training programme. What I have realised is that majority of TSI members are indifferent to the activities of the TSI. I appeal to the TSI members to be more proactive and become fellow members. The TSI requires more mature TSI members as executive committee.
In future Telemedicine will grow rapidly and we, the TSI, need to be very clear in what we advocate about teleconsultations. Documentation of Teleconsultations is of paramount importance. TSI needs to shift the HQs to the NCR and start a Telehealth education wing.
Please ensure positive participation in all TSI activities.
The New President Speaks

Col (Dr) AshviniGoel (Retd.)
President, Telemedicine Society of India
As I done the unenviable mantle of the President of Telemedicine Society of India, I cannot help but reflect upon the year gone by. It has indeed been a year that no one will forget in a hurry. Some notable events of the past year being; the TELEMEDICON 2019 organised at Indian Spinal Injuries Centre in New Delhi with the largest gathering of very senior government functionaries in any TSI conference so far; the proclamation of Govt support for ‘Regulatory Framework for the Practice of Telemedicine in India’; the hurried and intense work on the Draft Telemedicine Practice Guidelines by a small group of dedicated and sincere TSI members with legal background at behest of the Chairman Board of Governors MCI and Member NITI Aayog; the issuance of the “Telemedicine Practice Guidelines” for RMPs on 25th March 2020 quickly followed by similar guidelines for ASU practitioners by CCIM on 7th April and for Homeopathy practitioners by CCH on 10th April 2020; the quick and successful response by a committed group of TSI members in forming the Training Team and conducting ‘Online Basic Orientation Course on Telemedicine Practice Guidelines’, training a large number of doctors (RMPs) by curating content equalling global standards, mostly working ‘pro bono’; the havoc created by Covid Pandemic; the disruption of the daily life and acceptance of the ‘New Normal’; the ‘feeling of being in doldrums’ at the realization that we may have to forego TLELEMEDICON 2020 this year; the serendipitous decision by the Immediate Past President and the undersigned to approach a State Chapter of TSI (or a group of more than one) to organise the conference on a Virtual mode; TN Chapter taking up cudgels under the capable leadership of its President and the resulting stupendous success of the TELEMEDICON 2020.
The hurried melange of activities has left an indelible impression on my mind and possibly helped to shape my thoughts for the future. I wish to take this opportunity to share my thoughts with you all. As with all such endeavours, there is a great deal of subjectivity. Many of the thoughts and ideas are offshoots of observations over the past twenty years. If we attempt most, accomplish some and others do not see the light of the day; I think we would have done our job of doing a sincere effort of getting our Society on an even keel. Getting the process started and making it a self-sustaining process is what we must ensure.
In our consolidated effort to move forward as a society, there are a few housekeeping matters which require to be streamlined. A notable few being: manpower concerns within the society; financial avenues for sustaining the capacity building programs initiated by the society; partnering with other associations, industrial bodies as a matter of public outreach exercise; review of internal milieu, organisational restructuring. In order to achieve the foregoing, I intend to realize the following:
1.Implementing agile and decisive decision making: Implementing agile and decisive decision making within the Executive Committee and beyond the closed group, to ensure no new partnering initiative or moot point is side-lined: The entire world has now woken up to the benefits of Telemedicine technology after the advent of Covid pandemic. This has resulted in all and sundry jumping onto the Telehealth bandwagon with the majority of them being hard core profit oriented business entities well entrenched in cut-throat business and “for-profit” ethos. If we at TSI, want to have a place in this eco-system, we will have to follow a process of rationality in our thought process, well-researched and well-informed decisions and most importantly agile and decisive decision making.
2.Inclusive and participative governance of TSI activities: By office bearers, and other senior members who have been spearheading the cumulative efforts of the society over the years. TSI is now almost 800 members strong, and growing day by day in strength. I feel it is far too ambitious to think that an Executive Committee of 14 members comprising of COO, Immediate Past President, President, President Elect, Vice President, Secretary, Jt.Secy& Treasurer and the seven EC members; can do justice to all the decision making required to make TSI a globally recognized think-tank and promoter for Telehealth activities, especially when we are competing with organisations like ATA, HIMMS and other similar entities in the field of digital health. Hence, to be able to fulfil our obligations we need to reach out to all our members, especially the senior members, the TSI Margdarshaks to seek their views and recommendations in a process of participative governance. A number of committees have been constituted recently to enable this, and I exhort all TSI members to take this responsibility with all seriousness and in the right spirit to help steer TSI on the path of progress of being ‘Numero Uno’ in the field. I request that more and more members seek to be involved with the various committees that have been formed for ‘governance’ of TSI matters.
3.Growth and empowerment of Regional chapters: By supporting them financially, as well as extending institutional support, as and where required, to increase outreach, and make telemedicine available to the last mile. The Regional Chapters are the functional arms of The Society. The growth and empowerment of the Regional Chapters will go a long way towards progressing the agenda of The Society. I request all TSI members to explore avenues of growth within the spheres of influence of their Chapters. I promise that as President TSI, I will extend all support for all such activities.
4.Explore reasons for lack of involvement by TSI members in TSI activities: Remove any hurdles for involvement of TSI members in TSI activities, increase participation for inclusive growth of the society and its members. See para 3 above;
5.Increase membership: Increase membership both at individual and institutional levels; “each one, get one” is a strategy which could be adopted by us all to ensure that the opportunity which has been presented this year is not lost and we attempt to gainfully utilize this ‘God given’ opportunity to maximal benefit for The Society;
6.Revision of Bylaws: Revision of Bylaws is necessitated as the present are antiquated and must be aligned with the change in the overall ethos pertaining to the field of Telehealth, growing participation of the private sector, and other industry associations as well as NGOs seeking an alignment with TSI in augmenting the vision and activities of The Society;
7.Lateral linkages: In order to grow in this rapidly progressive field of Telehealth, TSI has to strike synergistic liaisons with other NGOs and industry majors who are functioning in this field. Lateral linkages with the industry and other agencies were forthcoming in plenty, however the various MOUs could not be finalised due to internal misgivings and apprehensions of some EC members. Our intention should be to streamline the internal processes for engaging in such partnerships to the betterment of The Society and to keep the momentum going;
8.Financially sustainable activities: Financially sustainable activities for the purposes of ensuring growth and smooth functioning of the society will go a long way towards fulfilling the aims and goals of The Society.
9.Training with Certification: Training with certification will have to be promoted to ach.ieve the goal set out by the Member, NITI AAYOG and in conformity with the Telemedicine Practice Guidelines for evangelizing telemedicine and accurate adoption of the Telemedicine Practice Guidelines by the community;
10.TSI website: Website of an organisation is its face that the visitors look at for the first time while enquiring about its activities, “first impressions are lasting impressions”. TSI website must be updated continuously to reflect the activities of the society, as well as to keep the community abreast with the latest updates from around the world;
11.TSI eMagazine/Journal: TSI eMagazine/Journal has to be rolled out on a defined, periodic basis, with high quality scientific content, demonstrating the commitment of the society to the cause of telemedicine;
12.Liaison with Govt functionaries: Sustained liaison with the concerned Govt functionaries, both at Centre and State level, in furthering the regulatory and policy work in the domain and practice of telemedicine;
13.Relocation of TSI HQ: Relocation of TSI HQ to NCR to facilitate convenience in conversations with the centre;
14.Development of Telehealth Standards and benchmarking capabilities: Development of Telehealth Standards, alongside government agencies, private bodies, and other designate agencies in collaborative efforts. Also, developing bench marking capabilities for Telehealth apps and platforms, by engaging with the industry and by advising and consulting within the society, leveraging the cumulative experience of the members from different walks of professional life;
15.Restructuring TSI as a corporate body: Restructuring TSI on lines of ATA/HIMSS ( Healthcare Information and Management Systems Society), which work in close contact with the Government, private players and take pride in operating as corporate bodies.
As a way forward, I invite participation of one and all, in the smooth functioning, promotion and activities of Our Society. Stay Safe, Stay Healthy.
TELEMEDICON2020 Stats
The registration fee for delegates was a meagre token amount to get their valuable commitment to attend and enjoy the 3 days of virtual technical feast.
The registration was slow to start but gradually towards the end touched 1126
Delegates – 923
Speakers, Chairpersons and Moderators – 203
Overall – 1126
Further breakup showed that the registrations included:
TSI member Registration – 220
Doctors – 586
Students 154
We had a small participation from the industry with about a dozen sponsors who were provided with a stall in the Virtual Exhibition hall.
The scope of the conference enlarged as the dates got closer. Finally we had almost 24 hours of conference time that were spent in three concurrent sessions on day two and three, making it almost 52 hours of deliberations on Telehealth. There were 18CME’s, Symposiums and Workshops including a Hackathon.
All the sessions have been video-recorded and we hope to make it available to all the members.
Claim Credit Hours for Attendance to TELEMEDICON 2020
The doctors who attended and submitted their medical registration numbers of council would be able to claim four credit hours from the Maharashtra Medical Council. Though the time was short but this was made possible due to the efforts of Dr. B.S. Ratta, Co-Chairman of the meeting. This made TELEMEDICON 2020 truly an academic meet.
TELEMEDICON2020 – A Summary of the Event

Bagmisikha Puhan
Executive Member, TSI
TELEMEDICON2020 was a new experience in this new normal. To encapsulate 52 hours of deliberations of the virtual meet would be impossible. However we would like to highlight few key takeaways from the event as this difficult year 2020 comes to close.
1.With the introduction of the legal framework, the trust in the ecosystem has been supplemented,and has fostered faith in the practitioners, patients, and the other valuable stakeholders in the ecosystem, in terms of care delivery.
2.In terms of rural health vis a vis telemedicine, reaching the last mile would require greater public-private participation; it is felt that increased interactions between the practitioner and the patients will increase the faith restored by the patients in the infrastructure. The government’s plans are laudable through its various projects to reach the last mile to deliver health to the masses using telehealth, however there are likely to be huge implementation challenges.
3.There is apprehension in the minds of the practitioners, in terms of the incumbency to comply with data privacy and protection laws.
4.Integration of the patient’s health / medical records in a centralized system would enable the practitioners to access documents from secure servers without having to concern themselves with storing the same onto their local servers and exposing themselves to additional risk.Furthermore, lack of clarity in respect of the retention timelines may lead to potential lapses on part of the data fiduciary / custodian with respect to data storage principles.
5.Training and capacity building exercises will have to be amplified, to bring the practitioners up to speed with the advanced technology, as well as the regulatory norms which they must adhere to in terms of delivery healthcare via means of information and communications technology (ICT).
6. In the face of the ongoing pandemic of Covid-19, the practicing physicians (from across several clinical specialties) have had to attend to a diverse spectrum of ailments via telemedicine consults; in doing so, they feel, the lists of medicines which are referred to within the TPG are limited and restrict the physician from managing the patient effectively / desirably. While the potential for abuse of medication/ drugs is relevant, the restrictions on drugs which can be prescribed over a telemedicine consult, undermines the very purpose of digital health, which is to widen the outreach, and serve the underserved.
7.There were deliberations with respect to the benefits of telemedicine, in reaching out to the vulnerable population in augmenting the mental health care infrastructure. The mental health practitioners have realized the benefits of telemedicine, which allows women, elderly, and home-bound citizenry to reach out to them for consultations. TPG has given the necessary fillip to the home-bound citizenry to access mental health professionals, without having to worry about their privacy, or their prowess to access such services, as and when necessary.
8.Deliberations were also made with respect to the minor/ children/ adolescent population, who are benefiting from access to mental health practitioners from across the vast geographical spectrum, without exposing themselves to the undue / unwarranted / unsupported physical visit to the practitioner/s.
9.The specialists have also witnessed a boost to their consultancy services and have been able to engage with the treating physicians, who may be situated in a poorly accessible demographic landscape (Tier-3 cities, remote areas).
10.Several practitioners have also brought to the fore, the challenge in spending a longer time in ‘raw data-entry’, especially the ones who are not conversant with the technology at hand. This leads to delay and extends the average discussion/ consultation time with the patient, adding to the already disparate physician-to-patient ratio in the country.
.11.A solution-oriented approach, leading to introduction of homogenous/ interoperable systems would be preferred.
12.Greater involvement of ancillary workers in supporting the physicians, patients, and other stakeholders in the ecosystem, is the need of the hour.
13.Practo in collaboration with TSI released a position paper, emphasizing on the gaps in the system and the overbearing positive implications of the new regulations. The paper highlights the associated statistics and the key levers in the ecosystem.
To surmise, during the conference, while the above factors were discussed, the participating delegates and faculty have expressed their gratitude to the government in enabling the ecosystem to flourish by way of the introduction and successful implementation of TPG.
The participation from dignitaries situated outside the country, brought to the fore, that as a society we have along way to go in terms of imbibing the practice of telemedicine in our daily lives. There is a pressing need to build the confidence in the patients to favor the practice and adoption of telemedicine, which is critical tosupport the lifestyle medicine practice, moving us from illness to wellness. Also, with the necessary capacity building and structured trainings, the practitioners will be able to become better aware of the telemedicine related laws and be more confident in their use of ICT in healthcare. A study presented by a French practitioner, showed that the numbers featuring the willingness to imbibe telemedicine practice have only risen since the country first introduced the legal framework over a decade ago. For India, while the geography and the demography pose challenges, there is also an invaluable opportunity presented by the onset of the pandemic, which is changing the perspective of the larger population, and reassuring faith in ICT for delivery of services.
This document only lends a very brief, high-level insight to the lengthy and engaging discussions during the conference; however, it brings to the fore the pressing needs, and the positive feedback since the release of TPG, and the continued practice of telemedicine through decades. We expect the healthcare fraternity to adopt ICT and augment their practices, as well as the patients to feel safer in interacting with their physicianstranscending physical barriers.
TELEMEDICON2020 – Free Papers and their Winners
There were 34 free papers submitted of which 27 were presented. There were thirteen podium and fourteenposters presentations.
Six Podium papers were selected as winners for best papers and will be issued certificates and cash award
These were as follows:
PODIUM WINNERS
1.Dr Sarang Patil, MUHS Nashik
Tele-pulmonology a ray of hope in elderly COPD patients
2.Moaz Hamid, Western Sussex Hospital, UK
Mobile Health Apps: Using the Five-Factor Model of Personality as a predictor of the preference for gamified features and their usage characteristics
3.Govinda Narke, Free Asthma Clinic Hadpsar Pune
Use of telemedicine for asthma control and follow up consultation during COVID pandemic
4.Akhila Kosuru, Deputy General Manager, Apollo Tele Health Services, Hyderabad
Perception of doctor for prescribing drugs in teleconsultation
5.Ms Jinchu Paul, NIMHANS, Bangalore
Effectiveness of the addition of virtual NIMHANS ECHO tele-mentoring model for skilled capacity building in providing quality care in alcohol use disorders in DMHP districts
6.Dr Avinash T,, Kidwai Memorial Institute of Oncology, Bangalore
Roadmap to paediatric oncology palliative care services through Telemedicine.POSTER PRESENTATION WINNERS
First
Aditi Kini, HCG Hospital
Feasibility of Tele-rehabilitation of swallow and communication & Functions–
Second
Zeenat Fatima, AIIMS, Bhopal
Feasibility and acceptability of Teleconsultation through video mode for diabetes at a tertiary care centre in India
Third
Vijayalakshmi Poreddi, NIMHANS Bengaluru
-Nursing Interns perceptions of Telenursing Implications
TELEMEDICON2020 Feedback
![]()
TELEMEDICON2020 – ‘Picture that Said It All’
TELEMEDCION2020 was attended by at least four speakers who were suffering from active COVID19 infections. COVID infection did not deter them from participating in this virtual meet. In fact Mr. Harish Manian, CEO of MGM Healthcare, Chennai spoke from his hospital bed about the Hospital Perspective for Tele-health Insurance.
| Mr. Harish Manian, CEO of MGM Healthcare, Chennai spoke from his Hospital Bed |
The next issue in Jan 2021 would carry the Part- 2 of TELEMEDICON2020 and cover the highlights of the various sessions
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter. |
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Design – Sankara Nethralaya
Technical Partner- www.medindia.net




 Telemedicine pRoject for screENing Diabetes and its complications in rural Tamil Nadu (TREND) project
Telemedicine pRoject for screENing Diabetes and its complications in rural Tamil Nadu (TREND) project Tele Counselling Solutions From Sankara Nethralaya
Tele Counselling Solutions From Sankara Nethralaya



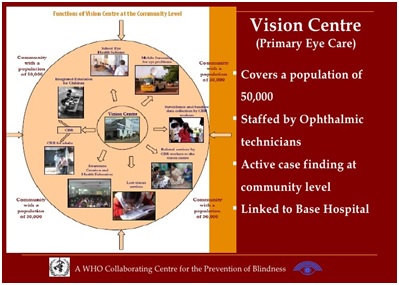 Vision centres, being closer to the community have a unique advantage to ensure treatment of chronic conditions are truly effective. Given that they are local to the patient, they are more accessible for regular follow up visits and can ensure patients stay on-track for their treatment. Aravind Eye Hospitals have ensured that patients with chronic conditions can procure medication and a patient registry helps to longitudinally monitor these patients over time.
Vision centres, being closer to the community have a unique advantage to ensure treatment of chronic conditions are truly effective. Given that they are local to the patient, they are more accessible for regular follow up visits and can ensure patients stay on-track for their treatment. Aravind Eye Hospitals have ensured that patients with chronic conditions can procure medication and a patient registry helps to longitudinally monitor these patients over time. Dr. N. Ramakrishnan AB (Int Med), AB (Crit Care), AB (Sleep Med), AB (Obesity Med), MMM, FACP, FCCP, FCCM, FAASM, FISDA, FICCM
Dr. N. Ramakrishnan AB (Int Med), AB (Crit Care), AB (Sleep Med), AB (Obesity Med), MMM, FACP, FCCP, FCCM, FAASM, FISDA, FICCM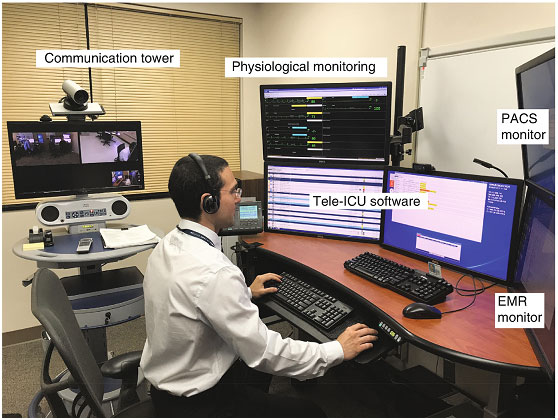 Chennai has been a leader in healthcare in our country and has several firsts to its credit. The first TeleICU anywhere outside the USA was a collaborative effort by Chennai Critical Care Services. We partnered with Advanced ICU Care, USA and started providing Tele-ICU for hospitals in America from 2010.
Chennai has been a leader in healthcare in our country and has several firsts to its credit. The first TeleICU anywhere outside the USA was a collaborative effort by Chennai Critical Care Services. We partnered with Advanced ICU Care, USA and started providing Tele-ICU for hospitals in America from 2010. In 2014, my colleague Adam Stepan and I began a project to develop original video and written case studies for a new hybrid MPA at the School of International and Public Affairs (SIPA) at Columbia University. We focused on innovations in providing essential public services such as police, fire, education, sustainable agriculture and health care. After considerable research, our innovation in health care focused on telemedicine and electronic record-sharing identified India as being at the cutting edge of that innovation.
In 2014, my colleague Adam Stepan and I began a project to develop original video and written case studies for a new hybrid MPA at the School of International and Public Affairs (SIPA) at Columbia University. We focused on innovations in providing essential public services such as police, fire, education, sustainable agriculture and health care. After considerable research, our innovation in health care focused on telemedicine and electronic record-sharing identified India as being at the cutting edge of that innovation.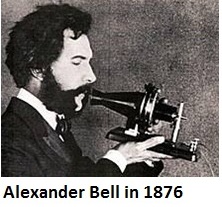 For doctors ‘Tele-consultations’ is nothing new. It started soon after the telephone was invented by Alexander Bell in 1876.Little do people know that the first call that Mr. Bell made was for medical help or for an emergency of sorts. Mr. Bell called his assistant Thomas Watson and said:
For doctors ‘Tele-consultations’ is nothing new. It started soon after the telephone was invented by Alexander Bell in 1876.Little do people know that the first call that Mr. Bell made was for medical help or for an emergency of sorts. Mr. Bell called his assistant Thomas Watson and said: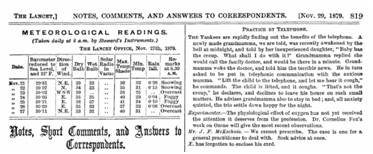 And on Nov’1879 another piece in Lancet spoke of Practice by telephone and its use that could bring down the visits to doctors clinics in the future.The commonest consultation on the telephone over the years perhaps has been – ‘Doctor I have a headache, what can I do.’
And on Nov’1879 another piece in Lancet spoke of Practice by telephone and its use that could bring down the visits to doctors clinics in the future.The commonest consultation on the telephone over the years perhaps has been – ‘Doctor I have a headache, what can I do.’
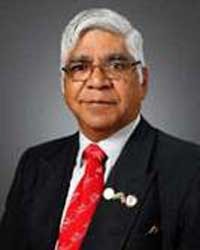 Telemedicine in India: Personal Reminiscences from 1996
Telemedicine in India: Personal Reminiscences from 1996
 Tele-Ophthalmology – in a COVID world – Opportunities and Challenges
Tele-Ophthalmology – in a COVID world – Opportunities and Challenges

 The most effective model during the COVID time for Ophthalmology was for follow up of patients such as Postoperative patients where advise was given on Medication changes, or Tele triage wherein patients were seen online and decision was taken if they have to come to Hospital or can be advised online, or even if they come to hospital which specialist they had to see and so on.
The most effective model during the COVID time for Ophthalmology was for follow up of patients such as Postoperative patients where advise was given on Medication changes, or Tele triage wherein patients were seen online and decision was taken if they have to come to Hospital or can be advised online, or even if they come to hospital which specialist they had to see and so on. Mobile Teleopthalmology
Mobile Teleopthalmology Best practices!
Best practices!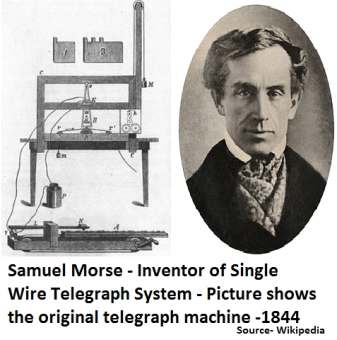 He went on to invent a single-wire telegraph system and the first Intercity public telegraph services were set up between Washington and Baltimore in 1844. In almost all the wars that followed the telegraph was used by the military to order medical supplies, transmit list of casualty and it is probable that some use of the telegraph in its early decades involved medical consultations.He was also the co-developer of Morse code that helped the commercial use of telegraphy. One of such codes was the internationally recognized distress signal SOS. The SOS letters were chosen because they are easy to transmit in Morse code: “S” is three dots, and “O” is three dashes.
He went on to invent a single-wire telegraph system and the first Intercity public telegraph services were set up between Washington and Baltimore in 1844. In almost all the wars that followed the telegraph was used by the military to order medical supplies, transmit list of casualty and it is probable that some use of the telegraph in its early decades involved medical consultations.He was also the co-developer of Morse code that helped the commercial use of telegraphy. One of such codes was the internationally recognized distress signal SOS. The SOS letters were chosen because they are easy to transmit in Morse code: “S” is three dots, and “O” is three dashes.