
Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
What is New?
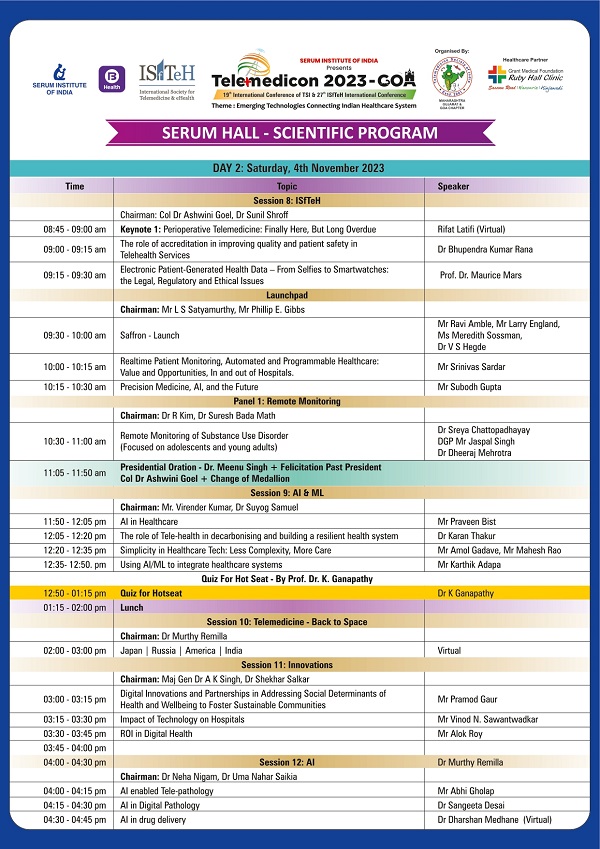
The month of October has been filled with celebrations. The TSI has successfully had its new amendment Bye-laws approved by the Registrars of Societies, addressing some past discrepancies. In the coming month, we will also see the installation of a new council. It’s noteworthy that this council has served for three years instead of the usual two, as specified in the old bye-laws.
We are now gearing up for TELEMEDICON 2023 in Goa, thanks to the efforts of Dr. Ratta and the Goa chapter of TSI. The program has been carefully planned, and we hope for a large turnout. Additionally, we continue to enjoy insightful contributions to our newsletter from Dr. Krishanga and Dr. Pavithra of Medindia.
Thank You
Dr. Sunil Shroff
Chief Editor
EC Member, TSI

TSI Byelaws 2.0
New Byelaws come into effect from Oct 04,2023
Dr. Murthy Remilla
Hony.Secretary TSI
Background:
As most of the members are aware, TSI has started functioning informally from the first Telemedicon Conference at Lucknow in 2001 and has been conducting annual conferences since then. However, the formal registration of the Society took place in May 2006 after a grand Telemedicon2005 at Bangalore under the aegis of ISRO.
Naturally like any society/organisation in its nascent phase of starting the activities, TSI had its simple Constitution & Byelaws registered in May 2006 with the primary objective of: “To promote and encourage development, advancement and research in the science of telemedicine and its associated fields”.
Over a period, many chapters have been formed in different states, many changes have taken place in the healthcare environment in the country, the technological arena across the globe which foretold the necessity to amend the style of operations and functioning of the Society including expansion of the society’s objectives and prescribing guidelines for Day to Day operations. Though some efforts were made in 2017 to go for some amendments, same could not be completed due to some technical reasons and loss of communication from RoS.
Keeping these and some other statutory requirements to align our practices to the written Byelaws and aligning the Byelaws to some of our traditional practices over two decades, TSI has taken up the task of amending the Byelaws to meet the society’s new ambitions, objectives and requirements of all the stakeholders.
This has been carried out through a series of EC meetings, National web meetings and taking as many suggestions and corrections as possible into account culminating in the final approval by Registrar of Society’s approval on Oct 04, 2023. Accordingly, the new Byelaws came into effect immediately and the same was notified to all the TSI members by email and through all WhatsApp groups.
However, it may be noted that this is a never ending process and any dynamic society has to keep its Byelaws and practices updated to meet the aspirations of the members.
Most importantly, in view of the long process and time needed to get any amendments in the Byelaws, it was decided to keep the Byelaws simple to the core and develop a separate TSI manual of Policies and Procedures.
Now, let’s have a glimpse at the major highlights of the changes that have been brought in through the current bye-laws –
1.The objectives have been expanded to embrace new practices and new technologies like:
- “To promote and encourage application of Telemedicine (TM) along with development, advancement and research in the field of Telemedicine/ TeleHealth/eHealth/Digital Health (which terms may be used interchangeably in different contexts) and associated fields; for improvement of overall Healthcare access”
- “To conduct regular scientific meetings, symposia, seminars and on matters related to digital health workshops”
- “To develop, co-ordinate and conduct knowledge and capacity building exchange programmes, with national/international organizations engaged in activities in the field of telemedicine.
- To work towards getting recognized as an accreditation body for Telemedicine/TeleHealth/eHealth etc.
- Spearheading or collaborating in the development of appropriate clinical and industry policies and standards, in view of adoption of and integration with TeleHealth.
2.Tenure of EC: The Tenure of the EC (Governing Body) has been amended to align with our practice as follows and the functions of all the office bearers have been elaborated to bring in more clarity and activity.
a. Immediate past president – One year
b. President – One year
c. President elect – One year
d. Vice-President – One year
e. Hony. Secretary – Two years
f. Jt. Secretary*- Two years
g. Treasurer – Two years
h. All other Executive Members – Two years (total seven in number)
i. COO: As per the terms, tenure and criterion if and when decided by the EC to appoint COO
* In tune with the recommendation of AGM 2021, the post of Jt.Secretary & Treasurer has been split into two separate posts of Jt. Secretary and Treasurer.
3.Membership types and fee: Two new types of Memberships – Associate Member for any non-graduate to become a member like a Life Member (except with the right to contest elections) & Oversees Institutional Members
4.A new clause on Cessation, Termination and Reinstatement/Re-admission has been introduced. Importantly to encourage the participation:
All National TSI Members upto the age 65 years should attend at least one National conference in personal/virtual mode in the previous Five Years, failing which their membership shall be suspended till their next participation in the annual conference
5.State Chapters: Since number of chapters is growing, the need to define their role and responsibilities; like fund generation and sharing percentage, preparing annual report, holding state chapter conferences etc. has been highlighted and decided to elaborate them in the TSI Manual of Policies and Procedures.
6.Auditor: The Executive Committee shall appoint and fix the appointment of an auditor and finalise the fee of the Auditor who shall be a Chartered Accountant at least once in three years.
7.Amendments: Any member of the society may propose amendments to the constitution/Byelaws by writing to the Hony. Secretary minimum 45 days before the GBM, who shall put up to the EC, if the EC approves the required change by majority, this shall be put up the Annual / Special GBM as required. Such amendment(s) may be amended by two-third affirmative votes of members present at the annual assembly, or where such affirmation has been provided via e-mails, facsimile, letter sent by courier or India Post, provided a copy of the proposed change has been circulated to each voting member 30 days in advance of the general body meeting. Such Amendments shall also be in accordance with the Societies Registration Act, 1860.
8.One clause on Fellowship Members though decided to be removed was inadvertently retained in the approved Byelaws and EC has approved to apply for removal of the same. The matter will be put up to the AGM for ratification and immediately after that ROS will be approached to issue a corrigendum.
9.Full version of the Approved Byelaws has been sent to each and every member of the society to registered email and WhatsApp Groups.
10.Request all Members to read, review and suggest any suggestion at any point of time without waiting for AGM or call for special meetings, which will be taken up by EC and put up for necessary processes.

AI with MRI can Recreate your Dreams
Dr. Krishanga Srivastava
Associate Editor, Medindia.net
Highlights:
Stable Diffusion AI re-creates images from brain scans, a breakthrough in visual perception
Incorporating photo captions into the algorithm enhances efficiency and reduces training needs
Potential applications range from understanding animal vision to aiding communication in paralysis
A new AI can create images based on what you dream. Scientists are trying to figure out how our brains translate what we see into mental images.
Now, a type of computer learning called Artificial Intelligence (AI) is improving at replicating this process. A recent study demonstrated that AI can analyze brain scans and generate images that closely resemble what a person saw. This could be used for various purposes, such as studying how different animals perceive the world or even recording dreams and assisting individuals who have limited mobility.
In the past, many labs utilized AI to analyze brain scans and generate images of things people had just seen, like faces or landscapes. This new study utilized a special AI program called Stable Diffusion, developed by a group in Germany and made public in 2022. It operates similarly to other AIs capable of generating images from text.
For this study, scientists in Japan added additional training to the Stable Diffusion program. They associated more words with thousands of photos and observed brain activity when participants viewed those photos during a brain scan study. This enhanced Stable Diffusion’s ability to comprehend the brain.
AI can Access Different Parts of the Brain to Recreate Dreams
The AI program utilizes information from various brain regions responsible for processing visual information, such as the occipital and temporal lobes. The system analyzes brain scans obtained using a specialized machine that indicates which parts of the brain are active.
When people look at a picture, the temporal lobes primarily register the content of the image (such as people or objects), while the occipital lobe mainly processes spatial arrangement, like their positions. This information is recorded in the brain scan, and the AI employs it to generate an image that resembles what the person saw.
In this study, scientists trained an AI algorithm called Stable Diffusion with brain scans from four individuals as they viewed a variety of photos. They reserved some of the scans for later testing, not using them in the training process. The AI initially generates random noise, akin to a TV screen fuzz, and then refines it into a clear image by comparing the person’s brain activity to the patterns learned during training. This results in an image that depicts the content of the photo and its spatial arrangement.
AI might be Good but not the Best
The AI performed well in representing spatial arrangements but struggled with objects like a clock tower. Instead of creating a clock tower, it generated something abstract. To address this, the scientists incorporated keywords from the photo captions. So, if a training photo featured a clock tower, the brain activity pattern would be associated with that object. Consequently, if the same pattern emerged in the testing phase, the AI would include the clock tower in the image. This refinement led to images that closely resembled the originals.
Reference: Brain Recording, Mind-Reading, and Neurotechnology: Ethical Issues from Consumer Devices to Brain-Based Speech Decoding
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7417394/
The AI underwent further testing with additional brain scans from the same individuals, producing accurate images of new subjects like a toy bear or an airplane. However, at present, it can only operate with scans from the individuals who initially trained it. Expanding its capabilities to work with other individuals would necessitate additional training. Nevertheless, this could signify a significant advancement in comprehending how our brains function and in generating images based on our thoughts and dreams.
“With further refinements, this technology could unlock a deeper understanding of our thoughts and dreams, and even shed light on how different species perceive the world.”

Telemedicine Needs Restructuring for Long-Term Sustainability
Dr. Pavithra
Assistant Editor, Medindia.net
Highlights:
The telemedicine, driven by the COVID-19 pandemic, has transformed healthcare in India
A 2023 report by TIFAC projects the Indian telemedicine market to grow significantly, with a 31% CAGR between 2020 and 2025, reaching USD 5.5 billion
India must evolve beyond doctor-patient calls, focusing on holistic, integrated care
The explosion of telemedicine occurred in the last four to five years, with a significant boost provided by the COVID-19 pandemic During the pandemic, teleconsultation platforms offered patients an alternative to in-person visits, helping them avoid the risk of contracting the virus in hospitals.
A Growing Market: Telemedicine in India
As we transition into the post-COVID-19 era, experts in the healthcare industry are noticing a decline in footfalls on telemedicine platforms compared to the peak activity during the pandemic.
While popular companies like Medindia, Practo, MeddiBuddy, MFine, and Lybrate continue to offer teleconsultation services, the landscape is changing.
According to a 2023 report by the Technology, Information Forecasting and Assessment Council (TIFAC), the telemedicine market in India is projected to experience significant growth, with a compound annual growth rate (CAGR) of 31 percent between 2020 and 2025, ultimately reaching a market size of USD 5.5 billion.
The increasing demand for teleconsultations, telepathology, teleradiology, and e-pharmacy services drives this expansion.
While the telemedicine market is poised for growth, independent teleconsultation companies are facing stabilization in their growth rates.
The rapid rise in telemedicine during the pandemic has given way to a more competitive environment, where large healthcare providers have gained the upper hand.
Dr. Vikram Venkateswaran from Deloitte India notes that telemedicine consultations now account for roughly 10 to 25 percent of total consultations at hospitals, with an average of around 10 percent. This plateau suggests that growth for independent teleconsultation services is slowing down.
The Need for an Integrated Telemedicine Approach
Industry critics argue that telemedicine needs to evolve to ensure sustainability and growth. Presently, many teleconsultation platforms primarily offer remote conversations between doctors and patients, lacking integrated care mechanisms that provide substantial value to patients.
Siddharth Srinivasan, CEO of Lupin Digital Health, believes that telemedicine should expand beyond mere doctor-patient calls. Patients should be able to measure their vitals at home, with real-time data accessible to their healthcare providers.
This holistic approach, where technology supports remote monitoring and diagnosis, is the way forward.
Dr. K Ganapathy, Director of Apollo Telemedicine Networking Foundation, emphasizes that despite fluctuations in footfalls, telehealth deployment has considerably increased compared to the pre-pandemic era. Hospitals, in particular, are actively integrating digital platforms to engage with patients, creating unique patient profiles, and offering personalized services.
Challenges in Telemedicine Implementation
While the growth of telemedicine in India is promising, there are still significant challenges to address. One critical concern is the digital divide. Not all patients have access to the necessary technology or a stable internet connection, especially in rural areas. Bridging this gap is essential to ensure equitable access to healthcare services.
Another challenge is data privacy and security. With the increasing reliance on digital platforms, protecting patients’ sensitive medical information becomes paramount. Telemedicine platforms must invest in robust cybersecurity measures and adhere to strict data protection regulations to maintain patient trust.
Additionally, there is a need for standardized protocols and guidelines for telemedicine practices. Establishing clear procedures for virtual consultations, remote monitoring, and prescription management can enhance the quality and consistency of care provided through telemedicine.
Regulatory Framework and Policy Considerations
A robust regulatory framework is imperative to govern telemedicine practices effectively. Policymakers must strike a balance between fostering innovation and safeguarding patient interests. Clear guidelines on licensing, reimbursement, and telemedicine ethics are essential to ensure that the sector operates ethically and efficiently.
Collaboration between the public and private sectors is also crucial. Government initiatives can play a pivotal role in promoting telemedicine adoption, especially in underserved regions. Public-private partnerships can facilitate the development of infrastructure and the deployment of telehealth services to remote areas.
Patient Education and Empowerment
Empowering patients with the knowledge and tools to actively participate in their healthcare is a vital aspect of telemedicine’s success. Educational initiatives can help patients understand how to use telemedicine platforms effectively, monitor their health indicators, and manage chronic conditions from the comfort of their homes.
Moreover, raising awareness about the benefits and limitations of telemedicine can help dispel misconceptions and build trust among patients and healthcare providers alike.
The consensus among experts is that telemedicine must play a more significant role in healthcare beyond consultations.
Dr. Venkateswaran points out that hospitals provide a care continuum, covering preoperative, operative, and post-operative care. While telemedicine platforms offer online consultations, they currently fall short of being an integral part of patient care.
To stay relevant and competitive, teleconsultation platforms are actively diversifying their services, moving beyond consultation-driven revenue models. They are exploring new solutions and interventions throughout the healthcare value chain, from patient engagement to digital outreach.
Emerging Technologies in Telemedicine
The future of telemedicine in India is intertwined with the rapid advancements in healthcare technology. Innovations such as artificial intelligence (AI), machine learning, and the Internet of Things (IoT) are poised to revolutionize how healthcare is delivered remotely.
AI-powered diagnostic tools can assist healthcare providers in making accurate assessments based on patient data and medical history. Similarly, IoT devices like wearable sensors and remote monitoring equipment enable continuous tracking of vital signs, providing real-time feedback to both patients and healthcare professionals.
Furthermore, virtual reality (VR) and augmented reality (AR) technologies hold immense potential in medical education and surgical planning. These immersive technologies can be leveraged to train healthcare professionals and enhance patient understanding of complex medical procedures.
In conclusion, the landscape of telemedicine in India is rapidly evolving, with both opportunities and challenges. The post-pandemic era has forced the industry to reassess its role and capabilities in the healthcare ecosystem.
As telemedicine grows, integrating with traditional healthcare services and providing value beyond consultations will be crucial for its long-term success.
References :
Advances in telemedicine in the 21st century
https://pubmed.ncbi.nlm.nih.gov/15366773/

Turning Data into Diagnosis: AI and ML to Transform PCOS Detection
Dr. Krishanga Srivastava
Associate Editor, Medindia.net
Highlights:
Artificial Intelligence (AI) and Machine Learning (ML) technologies are reshaping the landscape of women’s health
PCOS, a common hormone disorder, often goes undiagnosed or misdiagnosed
Integration of AI/ML into healthcare systems promises early PCOS identification and improved patient care
In the world of medical research, a digital transformation is taking place, set to reshape the landscape of women’s health. This change is powered by the boundless potential of artificial intelligence (AI) and machine learning (ML), casting a bright light on one of the most common yet often misunderstood conditions affecting women globally – Polycystic Ovary Syndrome (PCOS).
Artificial Intelligence and Machine Learning Join Hands to Combat PCOS
Artificial intelligence (AI) and machine learning (ML) have demonstrated notable efficacy in identifying and diagnosing Polycystic Ovary Syndrome (PCOS), the most prevalent hormone disorder affecting women aged 15 to 45.
This conclusion arises from a recent study conducted by the National Institutes of Health (NIH), where researchers systematically analyzed published scientific works employing AI/ML to scrutinize data for diagnosing and categorizing PCOS.
The findings underscore that AI/ML-based programs have shown considerable success in detecting PCOS. Dr. Janet Hall, a senior investigator and endocrinologist at the National Institute of Environmental Health Sciences (NIEHS) and a co-author of the study, emphasized the importance of this discovery, especially considering the widespread issue of under- and misdiagnosed cases of PCOS.
She stated that the effectiveness of AI and machine learning in detecting PCOS surpassed their initial expectations.
Why do Women get PCOS?
PCOS arises from irregular functioning of the ovaries, often accompanied by elevated testosterone levels. This condition can lead to irregular menstrual cycles, acne, excess facial or body hair, and hair thinning.
Additionally, women with PCOS face an elevated risk of developing type 2 diabetes, as well as various sleep, psychological, cardiovascular, and reproductive disorders, including uterine cancer and infertility.
Dr. Skand Shekhar, the senior author of the study, pointed out the diagnostic challenges associated with PCOS due to its overlap with other conditions. He highlighted the potential of integrating AI/ML into electronic health records and clinical settings to enhance the diagnosis and care of women with PCOS.
The study authors proposed amalgamating extensive population-based studies with electronic health data and analyzing common lab tests to pinpoint sensitive biomarkers that can facilitate PCOS diagnosis.
Diagnosis of PCOS relies on established standardized criteria, encompassing clinical features (e.g., acne, excess hair growth, and irregular periods) along with laboratory (e.g., elevated blood testosterone) and radiological findings (e.g., multiple small cysts and increased ovarian volume detected through ovarian ultrasound).
Nevertheless, because some PCOS features may co-occur with other conditions like obesity, diabetes, and cardiometabolic disorders, it often goes undetected.
How Can Artificial Intelligence and Machine Learning Help in PCOS Diagnosis?
AI refers to the utilization of computer-based systems to emulate human intelligence and aid in decision-making or predictions. ML is a subset of AI that focuses on learning from past events and applying that knowledge to future decisions. AI excels at processing extensive and diverse data, including that derived from electronic health records, making it invaluable for diagnosing challenging conditions such as PCOS.
It can aid in the following:
Improved Diagnosis: AI is proving to be highly effective in identifying and diagnosing PCOS. It can analyze a wide array of data, including clinical symptoms, hormone levels, and ultrasound images, leading to more accurate and timely diagnoses.
Early Intervention: AI enables early detection of PCOS, allowing for timely intervention and management. This is crucial in preventing associated health complications.
Personalized Treatment Plans: AI can analyze large datasets to create personalized treatment plans for individuals with PCOS. This tailored approach can lead to more effective outcomes.
Reduced Misdiagnoses: Due to its ability to process extensive and diverse data, AI can help mitigate the issue of under and misdiagnosed cases of PCOS, providing relief to many affected women.
Integration with Electronic Health Records: AI can be integrated into electronic health records, streamlining the diagnostic process and ensuring that healthcare providers have access to the most up-to-date information for effective patient care.
The researchers conducted a comprehensive review of peer-reviewed studies published over the past 25 years (1997-2022) that utilized AI/ML for PCOS detection. With the assistance of an experienced NIH librarian, they identified potentially eligible studies, ultimately screening 135 studies and incorporating 31 in their analysis.
All the studies were observational and evaluated the application of AI/ML technologies in patient diagnosis, with roughly half of them incorporating ultrasound images. The average age of the participants across the studies was 29.
Of the 10 studies that employed standardized diagnostic criteria for PCOS, detection accuracy ranged from 80% to 90%.
Dr. Skand Shekhar highlighted the study’s key finding, emphasizing the remarkably high performance of AI/ML in detecting PCOS across various diagnostic and classification methods.
The authors underscored the potential of AI/ML-based programs to significantly improve our ability to identify PCOS in women at an early stage, leading to cost savings and reducing the overall burden of PCOS on patients and the healthcare system.
They also noted that subsequent studies with rigorous validation and testing protocols will facilitate the seamless integration of AI/ML for chronic health conditions.
By combining state-of-the-art technology with unwavering human commitment, the diagnosis and treatment of PCOS are no longer shrouded in uncertainty but will be illuminated with exceptional clarity and accuracy.
Reference:
Application of Machine Learning and Artificial Intelligence in the Diagnosis and Classification of Polycystic Ovarian Syndrome: A Systematic Review.
https://www.frontiersin.org/articles/10.3389/fendo.2023.1106625/full


Telemedicine – News from India & Abroad
Can AI-Based Detection Prevent Heart-Related Complications?
Researchers at the Smidt Heart Institute at Cedars-Sinai have discovered that an artificial intelligence (AI) algorithm can identify atrial fibrillation…..Readmore
AI in Healthcare: Patients’ Comfort Tied to Familiarity
The degree of patients’ comfort with healthcare facilities employing artificial intelligence (AI) is found to be impacted by their familiarity with AI technology…….. Readmore
The Future of Storytelling With ChatGPT-4
According to two separate studies, OpenAI’s ChatGPT-4 has demonstrated an impressive ability to generate customized personal stories by tapping into stream-of-consciousness…..Reademore
Samsung Galaxy Watch Series Introduces Cutting-Edge Sleep Apnea Detection
Korea’s Ministry of Food and Drug Safety (MFDS) has granted approval for the sleep apnea feature within the Samsung Health Monitor app……Readmore
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
- Report can be from 500 to 600 words
- Report Should be relevant to Telemedicine or Medical Informatics
- No promotion of self or any product
- Avoid plagiarism
- All references should be included
- Provide any attributions
- Visuals are welcome including video links
- Send full authors name, degrees, affiliations along with a passport sized photograph of good resolution. If multiple authors only main author photo to be sent.
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net



























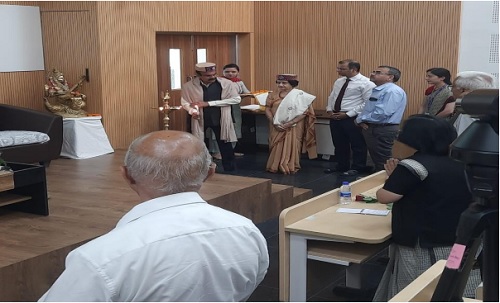






















 Faculty Empowerment Program on Telemedicine and Health Care Research
Faculty Empowerment Program on Telemedicine and Health Care Research







 DCGI issues notice to e-pharmacies for online sale of drugs without a license
DCGI issues notice to e-pharmacies for online sale of drugs without a license Satellite to Block Chain – A new paradigm in Covid care delivery through Telemedicine under India’s Health care Mission “Ayushman Bharat“
Satellite to Block Chain – A new paradigm in Covid care delivery through Telemedicine under India’s Health care Mission “Ayushman Bharat“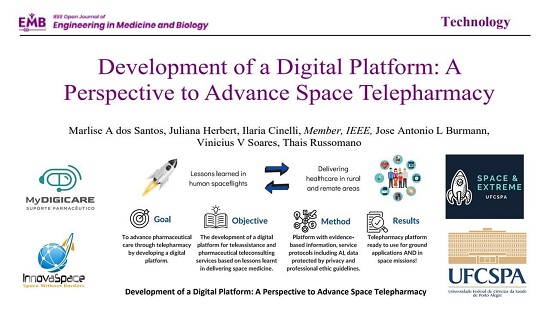

 Telemedicine Workshop for Trauma & Stroke
Telemedicine Workshop for Trauma & Stroke 



 Global Recognition received for Safe Delivery of Tele mental health services following legal and ethical Standards
Global Recognition received for Safe Delivery of Tele mental health services following legal and ethical Standards

 A Journey Into Space
A Journey Into Space
 Virtual healthcare in the new normal
Virtual healthcare in the new normal