Click Here to Download PDF Version

Telehealth Newsletter
Official Newsletter of Tamil Nadu Chapter of Telemedicine Society of India
|
What is New? This issue contains two important reports about the remarkable progress.made with Tele-ICU care during the ongoing pandemic. Tele-ICU is the best example of telemedicine not only saving lives but also making access to acute care possible in remote locations at an affordable cost. The average cost of care is atleast 50 to 60% less than the cost of care in a tertiary set up. However there are some challenges with the tele-ICU care as the current telemedicine guidelines falls somewhat short for this type of care and require more clarity on the regulations in areas such as the consent process and also provide a list of life saving medications that can be administered by remote trained health care workers (not RMPs) under the instructions of the ICU specialists. This empowerment will truly benefit the telemedicine ecosystem and the large rural population of the country. Thank You |
 Technology Transformation of Critical Care
Technology Transformation of Critical Care
Dr. Dhruv Joshi, M.D. ABIM (Pulmonary, Critical Care, Internal Medicine)
CEO & Co-Founder, Cloudphysician
Introduction
Cloudphysician is a healthcare delivery company that leverages technology to provide access to high-quality critical care to hospitals across the country using technology. Shortage of trained medical personnel and gaps in the delivery of high-quality critical care are a universal problem. Cloudphysician’s Care Center in Bengaluru is staffed 24/7 with a highly qualified and trained critical care team that includes trained intensivists, critical care nurses, pharmacologists and dieticians. The multidisciplinary clinical team uses RADAR, their smart ICU platform, to connect to hospital bedside teams in ICUs to oversee and manage the care of critically ill patients across multiple regions.
RADAR incorporates automation, communication, real time video, data analytics and AI/ML to help expert care providers connect to and improve the quality of care for patients.
Success stories
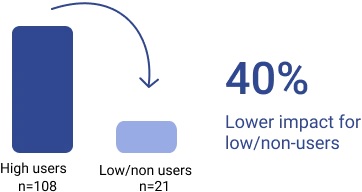
Hospitals served by Cloudphysician’s highly specialized team have seen an improvement in quality of care. For instance, a multispeciality hospital in North India collaborated with Cloudphysician to manage their patients. The hospital had a high patient intake and were facing difficulties with nighttime patient care. Cloudphysician tele-critical care team worked hand in hand with consultants and nurses at the hospital to provide quality and evidence based care. Availability of an intensivist 24/7, proactive monitoring and institution of quality protocols with respect to antibiotic usage, infection control practices and hand hygiene led to an improvement in patient outcomes including reduction of ICU mortality rate by half.
In another example at a multispeciality hospital in a tier 2 city in South India, an elderly woman was admitted with an altered level of consciousness. Her work of breathing (WOB) was very high, and she was immediately intubated and shifted to the ICU. An incorrectly placed endotracheal tube led to a collapsed left lung. The vigilant eye of the tele-critical care team immediately asked for an X-ray and picked up the incorrectly located tube, following which the intensivist immediately guided the hospital team to reposition the tube and re-expand the lung. Within 30 minutes of corrective actions the vital functions returned to normal. The collaborative effort saved the patient’s life who went on to make a full recovery.
National presence
Across 15 states in India, Cloudphysician has taken care of over 30,000 patients in critical care settings. To date, we have successfully equipped healthcare providers with advanced adult critical care support in not just multi-specialty hospitals but also medical and surgical focused single-specialty hospitals. The model is designed for easy adoption even in resource-constrained settings. We have collaborated with over 65 hospitals serving over 1000 ICU beds ranging from community hospitals in tier 1 cities like Bengaluru and Mumbai to hospitals in remote areas of Assam. The solution includes extensive upskilling and training programs. The clinical teams at our partner hospitals undergo regular upskilling programs allowing them to manage more complex critically ill patients and ensures better patient outcomes.
The model has resulted in the creation of centers of critical care excellence, where the partner hospitals have been able to serve the communities, reducing the need for patients to be transferred to other locations and making quality care more accessible for patients and their families. The 24/7 intensivist led vigilance and evidence-based treatment plans allow peace of mind for the hospital consultants and specialists. Overall, a reduction in medical errors was observed; better and faster response to emergencies and better implementation of protocols that are appropriate to the setting were seen.
Cloudphysician had onboarded 14 hospitals during the first and second wave of COVID-19 pandemic in India managing over 400 ICU beds. We have been a proud recipient of CAWACH grant from the Department of Science and Technology, GoI, for supporting COVID-19 response. We were also the finalists at Ayushman Bharat startup challenge and Market Access Program. For connecting COVID-positive ICUs during the second wave in India, we were felicitated by the Government of Maharashtra and the Maharashtra State Innovation Society.
About the author:
Dr. Dhruv Joshi is the co-founder and CEO of Cloudphysician. He trained in Pulmonary and Critical Care at the Cleveland Clinic Foundation, USA.


 eACCESS : Surfing the stormy waves of the pandemic
eACCESS : Surfing the stormy waves of the pandemic
Dr. Sai Praveen Haranath MBBS,MPH,FCCP
American Board Certified in Internal Medicine, Pulmonary and Critical Care Medicine
Senior Consultant Pulmonologist & Critical Care Specialist
Medical Director, Apollo eACCESS TeleICU Service, Apollo Hospitals, Jubilee Hills, Hyderabad, India.
The eACCESS program (Apollo Electronic Critical Care and Emergency Services) at Apollo Hospitals has been managing critically ill patients remotely for several years. During the COVID pandemic a rapid pivot was made to assist in COVID triage, monitoring and treatment of patients who were positive for the SARS-COv2 infection.
Patients all over India were evaluated for COVID symptoms using the same national consensus protocol to manage our bedside patients within the hospital group. Over 50 versions of the treatment plan were used as the evidence and science of COVID care evolved. Remote sites benefited from the advances instantly and knowledge sharing and transfer was immediate. While the eACCESS program managed traditional ICU patients, during COVID many new innovations were designed and tested. The ecosystem had the support and guidance of upper management and allowed the group to function in a nimble manner despite being a part of a large corporate hospital group with multiple stakeholders and processes.
There were three key areas that we focused on which allowed the concept of tele-ICU care to become socialized and accepted even in areas that had rudimentary critical care.
1. Education on critical care principles
2. Management of the spectrum of respiratory failure
3. Advanced consultation with coordination of escalation in care
Education of external non-Apollo remote sites as well as internal sites has been ongoing since the evolution of the tele-critical care program. During COVID this took on an urgency due to the rapid change in treatment protocols. Large public sector units required remote guidance for COVID triage and care. On a national scale we coordinated with the different units of Apollo Hospitals Group including remote care, bedside care, paramedics, lab services and information technology . Using this process we had regular didactic as well as on the job training of nurses, junior doctors and ancillary personnel located in over 27 locations around India.
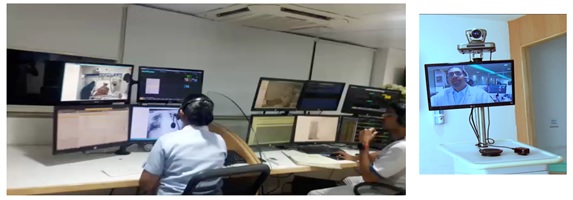
Almost 17,000 tele-critical care patients have been managed in one external hospital group alone. Internal monitoring of isolated COVID patients was also done for our own hospital system .The acuity of illness as expected fluctuated with the waves of the pandemic. Respiratory failure was widespread but many patients only required oxygen and titration of treatment based on oxygen saturation was made. Likewise evaluation of cause of hypoxia especially related to the possibility of coagulopathy was also done using point of care diagnostics. High flow oxygen titration, non-invasive ventilator initiation as well as adjustment of invasive ventilators were managed remotely. Using high fidelity cameras ventilator waveform troubleshooting was routinely done. Direct interaction with registered medical practitioners and nurses at the bedside has been an integral part of the process.
There were many remote sites with complex respiratory failure including ARDS with septic shock who had no prior experience handling such sick patients. Ad hoc rapid connectivity was established and triage for ECMO as well as stabilization prior to transfer was arranged. Several centres around India were able to save patients with expert help in evidence based critical care and standard of care measures. Many referrals were initiated by patient relatives themselves and eACCESS teams would contact the bedside providers for permission to virtually manage their patients in coordination with the existing team. Fortunately all locations were open to coordination and communication.
I bring up this point because the key to a successful tele-critical care program is open communication and redundant systems. In a traditional business development process there was a linear approach where remote sites or our program would discuss the feasibility and need for remote critical care. This required a certain amount of education and awareness at both sides. Remote doctors who were often the owners of the hospitals needed to see value that was financial as well as adding to the services provided from their site. Our program likewise had to understand the niche needs of each center and communicate this effectively.
The latest in this progressive remote care process has been the desire to reach out to as many smaller sites as possible to begin a process of improved equity in critical care access. With this in mind we have enrolled over 180 hospitals nationally with a comprehensive care model where critical care is one part of this engagement. Covering over 600 ICU beds the model seeks to be inclusive as well as cost efficient. The definition of critical care may need to change as patients may need intensive care anywhere, anytime. Using remote technology as well as a user friendly intuitive electronic medical record, we are now able to deliver world class care.
Our current focus is on standardization of care protocols and incorporating into workflows. We are also actively evaluating our outcomes and processes and trying to share our learnings through publications and other venues. The core value of delivering exceptional care to everyone is possible with remote care and especially remote critical care when lives are truly at stake. Doing this with empathy is an art and a skill that will be great to disseminate widely as the need is immense and immediate.
Reference:
1. https://www.apollohospitals.com/departments/critical-care/download-resources/news-letter/
2. https://www.theweek.in/theweek/cover/2022/01/15/apollo-hospitals-has-played-a-key-role-in-mainstreaming-telehealth-services.html
3. https://hlh.who.int/learning-briefs/electronic-intensive-care-units—a-model-of-critical-care-delivery
4. Haranath SP, Ganapathy K, Kesavarapu SR, Kuragayala SD. eNeuroIntensive Care in India: The Need of the Hour. Neurol India. 2021 Mar-Apr;69(2):245-251. doi: 10.4103/0028-3886.314591. PMID: 33904432.
 HTIC HEALTHCARE CONCLAVE – TELEMEDICINE
HTIC HEALTHCARE CONCLAVE – TELEMEDICINE
Reports By – Ms. Harshini & Ms. Sumithra
Lead Program Managers,
Indian Institute of Technology Madras, Healthcare Technology Innovation Centre
Email – impact@htic.iitm.ac.in
The HTIC Healthcare Conclave is conducted once in every quarter. The aim of this series is to bring successful entrepreneurs, Technical and Business experts from different domains under health care to share insights and to discuss the upcoming trends, Innovation, technologies, and bottlenecks. The conclave brings best minds in the medical and healthcare industry, to share the progress and the challenges in the different sectors.
The January 2022 conclave was conducted in collaboration with TSI – TN chapter, comprised of two panel discussions, two expert sessions and start-ups demonstrations in Tele Health. (see poster below)

A Keynote Address was delivered by Dr V Mohan, Chairman, Dr Mohan’s Diabetes Specialities Centre & Director, Madras Diabetes Research Foundation, Padma Shri Awardee in which he gave an overview on the Role of Telemedicine in Diabetes. The next part of the session included Panel Discussion on the topic Telehealth – Practitioner’s perspective and Patient experiences where we had diverse set of speakers from doctors to Startups, chaired by Dr T. Senthil, Founder & CEO, Welcare Health Systems Pvt Ltd. The panellists included Prof. K.Ganapathy, Member of Board of Directors. Apollo Telemedicine Networking Foundation & Apollo Telehealth Services, Dr.S. Dheeraj Krishnaa,Head Telemedicine-Star Health Insurance & Dr Dhruv Joshi, CEO & Co-founder, Cloudphysician. The discussion included the impact of Telemedicine in our day-to-day life and milestones that it must overcome for better performance. Further to that we had Expert Talks by Dr.Sunil Shroff, President, TSI TN Chapter, Senior Consultant Urologist & Transplant Surgeon and Prof Dr S.Natarajan, Chief Clinical Services & Chief Vitreo Retinal Services, Aditya Jyot Eye Hospital (A unit of Dr Agarwal’s Eye Hospital) Mumbai, President Teleophthalmology Society of India, Padma Shri Awardee on Understanding Telemedicine Requirements & Regulations and Teleophthalmology for Blind Free India respectively. The last part of the session included a panel discussion on the topic Innovation & Practices in Telemedicine chaired by Ms Padma Chandrasekaran, Angel Investor and Management Advisor. This panel was designed in a way to bring out the use of Telemedicine in various fields which included Radiology, Ophthalmology, ICU, ENT, etc. The panel included Dr Amit Gupta, Radiologist, Founder, AIRMED PATHLABS, Dr. T. Senthil, Founder & CEO, Welcare Health Systems Pvt Ltd, Dr.Sheila John, Head of Teleophthalmology, Sankara Nethralaya, Dr.Vidya Ramkumar, of Speech, Language & Hearing Sciences, Sri Ramachandra Faculty of Allied Health Science and Mr Harsha Muroor, Founder & CEO, Teslon Technologies Pvt Ltd. We also had start-up demonstrations where we had 4 start-ups to show a demo of their product to the crowd.
The Conclave gave an overall view on how the pandemic has changed life digitally and adoption in healthcare in Telemedicine.
 Rights of Patients vs. Rights of Doctors in Online Consultation
Rights of Patients vs. Rights of Doctors in Online Consultation
Anay Shukla
Founding Partner, Arogya Legal – Health Laws Specialist Law Firm
Saloni Kedia
Associate, Arogya Legal – Health Laws Specialist Law Firm
Telemedicine was measured experimental few years ago but with the progression in technology it is a reality today. However, it has its own shortcomings. One of the crucial hurdles is the lack of awareness and certainty of rights amongst the patients and doctors in the practise of telemedicine. Both the patient and the physician are unclear about the standard of care to offer and how to defend his or her rights when using telemedicine. Below given are some of the rights that can be exercised by patients and doctors while interacting.
Patient and doctor identification
During the first consultation with the doctor, the doctor has a right to verify the patient’s identity to his or her confidence by asking for the patient’s name, age, address, contact, email address or any other relevant identification. However, the same is not required under a follow-up teleconsultation but, if in question; the doctor should authenticate the patient’s identification, just as he or she did during the initial visit.
Moreover, it is also the duty of the doctor to inform patient of his/her identity and qualifications before beginning any teleconsultation which in turn is the absolute right of the patient to identify the credibility of the treating doctor.
Right to choose the appropriate mode of consultation
For patient consultation, a doctor can choose any medium as a matter of right. However, before commencing with the teleconsultation, the doctor should use his or her prudent judgement to determine if such medium is suitable and in the patient’s best interests. Although patient has complete right to opt for teleconsultation, but it is again the right and liberty conferred to doctor to choose the appropriate medium for teleconsultation and decide whether to evaluate the patient in person or remotely on case to case basis.
Right to second opinion and discontinuance of teleconsultation
The patient has an absolute liberty to go for second opinion for the line of treatment or diagnosis offered by the treating doctor and the treating doctor has no authority to question for the same. Further, the patient also has a right to discontinue the teleconsultation at any time if they wish to do so.
Right to access to relevant medical information
The doctor has a complete right to ask for pertinent information from the patient during the teleconsultation before making any diagnosis or treatment decision. On the other hand, it is the patient’s duty to provide enough correct information to the doctor as it is the patient who will be accountable for the authenticity of the information exchanged with the doctor. Moreover, the doctor also has right to obtain additional medical information from the patient during the course of treatment if needed.
Patient’s sensitive data and consent
It is patient’s right to have its personal sensitive medical information to be protected when shared with doctor during teleconsultation. The doctors as a mandatory obligation should never divulge or share any patient’s information with any third party without the patient’s prior written consent.
Right to verification of the Caregiver
Before giving teleconsultation for a minor or incapacitated person, the doctor has a right to verify the caregiver’s identification and authorisation by way of any signed authority letter given by the patient or his/her legal representatives or any government proof that verifies patient’s relationship with the caregiver for ethical teleconsultation and in the best interest of the patient.
Rights under emergency situation
Needless to mention, it is the right of the patient to have access to teleconsultation in emergency situation. However, this mode can only be used if it is the only method to deliver timely care. Further, it is also the right inferred to the doctor to restrict its emergency teleconsultation to first aid, life-saving procedures, counselling, and referrals thereby giving recommendation or directive to the patient or his/her caretaker to check with the doctor in person as soon as possible.
Right to prescription, invoice and fees
The doctor has a right to charge for Tele-consultation at a reasonable rate and in turn it is the right of the patient to have a receipt or invoice issued in exchange of the fees. The patient also has the implied right to have appropriate prescription from the treating doctor with respect to diagnosis, treatment or medication, if any.
Cabinet approves implementation of Ayushman Bharat Digital Mission with a budget of Rs.1,600 crore for five years
Highlights:
- ABDM will improve equitable access to quality healthcare by encouraging use of technologies such as telemedicine and enabling national portability of health services
- Citizens will be able to create their ABHA (Ayushman Bharat Health Account) numbers, to which their digital health records can be linked
The Union Cabinet, chaired by Prime Minister Shri Narendra Modi has approved the national roll-out of Central Sector Scheme, Ayushman Bharat Digital Mission (ABDM) of Ministry of Health and Family Welfare, Government of India, with a budget of Rs.1,600 crore for five years. The National Health Authority (NHA) will be the implementing agency of Ayushman Bharat Digital Mission (ABDM).
Digital health solutions across healthcare ecosystem have proven to be of immense benefit over the years, with CoWIN, Arogya Setu and eSanjeevani further demonstrating the role technology can play in enabling access to healthcare. However, there is a need to integrate such solutions for continuum of care, and effective utilization of resources.
Based on the foundations laid down in the form of Jan Dhan, Aadhaar and Mobile (JAM) trinity and other digital initiatives of the government, Ayushman Bharat Digital Mission (ABDM) is creating a seamless online platform through the provision of a wide-range of data, information and infrastructure services, duly leveraging open, interoperable, standards-based digital systems while ensuring the security, confidentiality and privacy of health-related personal information.
Under the ABDM, citizens will be able to create their ABHA (Ayushman Bharat Health Account) numbers, to which their digital health records can be linked. This will enable creation of longitudinal health records for individuals across various healthcare providers, and improve clinical decision making by healthcare providers. The mission will improve equitable access to quality healthcare by encouraging use of technologies such as telemedicine and enabling national portability of health services.
The pilot of ABDM was completed in the six Union Territories of Ladakh, Chandigarh, Dadra & Nagar Haveli and Daman & Diu, Puducherry, Andaman and Nicobar Islands and Lakshadweep with successful demonstration of technology platform developed by the NHA. During the pilot, digital sandbox was created in which more than 774 partner solutions are undergoing integration. As on 24th February 2022, 17,33,69,087 Ayushman Bharat Health Accounts have been created and 10,114 doctors and 17,319 health facilities have been registered in ABDM.
Not only will ABDM facilitate evidence-based decision making for effective public health interventions, but it will also catalyse innovation and generate employment across the healthcare ecosystem…Read More
Telemedicine – News from India & Abroad
India
Ayush Ministry Gets Rs 3,050 Crore in Union Budget FY23
Ayush Ministry has been allocated about Rs 3,050 crore this year in the Union Budget 2022-23. The Budget 2022-23 was presented by Union Finance Minister Nirmala Sitharaman on Tuesday. The budget allocation will help the Ayush in the upgradation of its hospitals and dispensaries…..Readmore
Indian Government Mandates QR Codes for Drug Packages
Indian government has made QR (quick response) codes mandatory on packages of drug manufacturing ingredients to crack down on fake medicines. The Union health ministry gazette notified guidelines, saying “every active pharmaceutical…Read More
International
Artificial Intelligence (AI) — Future of Neurosurgery?
Technical performance and learning outcomes during simulated brain tumor removal may be enhanced by artificial intelligence (AI) as per a study at the Neurosurgical Simulation and Artificial Intelligence Learning Centre at The Neuro (Montreal Neurological Institute-Hospital,…Read More
Advancements in Facial Recognition Technology
Neural processing techniques allowed capturing three facial expressions by triggering actions in a VR setting as per a study published in the International Journal of Human-Computer Studies. Our face can unlock a smartphone, provide access to a secure building…Read More
Click here to Become a Member of Telemedicine Society of India
Telemedicine Practice Guidelines – A Foundation Course for RMPs by TSI Faculty
To know more about the Telemedicine Foundation Course click on the link below:
https://tsitn.org/tpg-course/
TN – TSI invites all the TSI Chapters and Members to submit information on their upcoming Webinar or Events (50 words), News related to Telemedicine (200 words) or short articles (500 words) for the monthly e-newsletter.Guidelines for submission to TN TSI Newsletter-
|
Submission may be sent to – tsigrouptn@gmail.com
Editors reserve the rights for accepting and publishing any submitted material.
Editor in Chief – Dr. Sunil Shroff
Editors – Dr. Senthil Tamilarasan & Dr. Sheila John
Technical Partner- https://www.medindia.net








 A model for sustainable, partnership-based telehealth services in rural India: An early process evaluation from Tuver village, Gujarat
A model for sustainable, partnership-based telehealth services in rural India: An early process evaluation from Tuver village, Gujarat